Fillable Printable OPM Form 2809
Fillable Printable OPM Form 2809
OPM Form 2809
Health Benefits Election Form
Form Approved:
OMB No. 3206-0141
Who May Use OPM Form 2809
•
Annuitants retired under the Civil Service Retirement System
(CSRS) or Federal Employees Retirement System (FERS)
•
Survivor annuitants under CSRS or FERS
•
Former spouses
•
Children and former spouses who are eligible for temporary
continuation of coverage
Instructions for Completing OPM 2809
Type or print firmly.
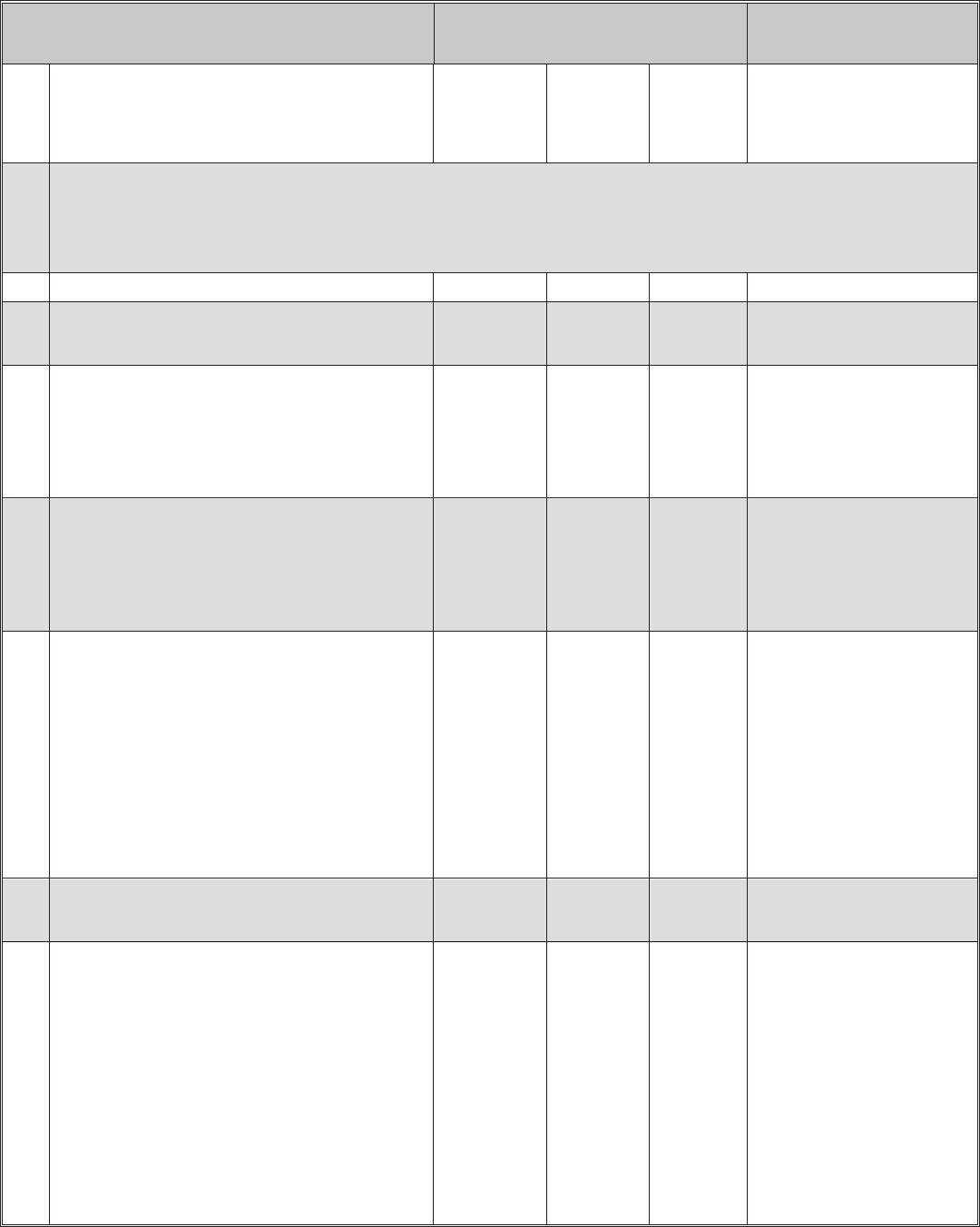
Part A — Enrollee and Family Member Information.
You must complete this part.
Item 1. Enter your legal name.
Item 2. Provide your Social Security number.
Item 3. Enter your date of birth.
Item 4. Enter your sex.
Item 5. If you are separated but not divorced, you are still married.
Item 6. Enter your emailing address.
Item 7. If you have Medicare, check which Parts you have, including
prescription drug coverage under Medicare Part D.
Item 8. If you have Medicare, enter your Medicare Claim Number.
This number is on your Medicare card.
Item 9. If you are covered by other health insurance (private, state,
Medicaid, Peace Corps, TRICARE, CHAMPVA, or another
FEHB enrollment), either in your name or under a family
member’s policy, check yes and complete item 10.
TRICARE is a health care program for active duty and retired
members of the uniformed services, their families, and
survivors. This includes TRICARE for Life for members age
65 and older.
Item 10. Select or write the name of any other insurance that covers
you.
Item 11. If applicable, provide your email address.
Item 12. Provide your day time telephone number.
If your enrollment is for Self and Family, complete information for your
family members. (If you need extra space for additional family members,
list them on a separate sheet and attach.)
The instructions for completing items 13 through 24 for your initial
family member also apply to the information you provide for additional
family members in items 25 through 48.
Item 14. Please provide Social Security numbers for your dependents,
if they have one. If your dependents do not have Social
Security numbers, leave blank; benefits will not be withheld.
(See Privacy Act Statement on page 4.)
Item 15. Provide the date of birth of the family member.
Item 16. Provide sex of family member.
Item 17. Provide the code which indicates the relationship of each
family member to you.
Code Family Relationship
01
Spouse
19 Child under age 26
09
Adopted Child
17 Stepchild
10 Foster Child
99
Disabled child age 26 or older who is incapable of self-support
because of a physical or mental disability that began before his/her
26th birthday.
Item 18.
If your family member does not live with you, enter his/her
home address.
Item 19. If a family member has Medicare, check which Parts he/she
has, including prescription drug coverage under Medicare
Part D.
Item 20. If your family member has Medicare, enter his/her Medicare
Claim Number. This Number is on his/her Medicare card.
Item 21. Indicate whether the family member has health coverage
other than Medicare.
Item 22. If a family member has TRICARE (see item 9), or other
group insurance (private, state, Medicaid, Peace Corps, or
another FEHB enrollment), check the box. Give the name and
policy number of any other insurance this family member
has.
Item 23. Enter email address, if applicable, for your spouse or adult
child.
Item 24. Enter the preferred telephone number, if applicable, of your
spouse or adult child.
Family Members Eligible for Coverage
Unless you are a former spouse or survivor annuitant, family members
eligible for coverage under your Self and Family enrollment include
your spouse and your children under age 26. Eligible children include
your legitimate or adopted children, step children, recognized natural
children, or foster children, who live with you in a regular parent-child
relationship.
Other relatives (for example, your parents) are not eligible for coverage
even if they live with you and are dependent upon you.
If you are a former spouse or survivor annuitant, family members
eligible for coverage under your Self and Family enrollment are the
natural or adopted children under age 26 of both you and your former
or deceased spouse.
OPM Form 2809
Previous editions are not usable.
1
Revised December 2013
In some cases, a disabled child age 26 or older is eligible for coverage
under your Self and Family enrollment if you provide adequate medical
certification of a mental or physical disability that existed before his/her
26th birthday and renders the child incapable of self-support.
Note: The Office of Personnel Management can give you additional
details about family member eligibility including any certification or
documentation that may be required for coverage.
Part B — FEHB Plan You Are Currently Enrolled In.
You must complete this part if you are changing, canceling, or
suspending your enrollment.
Item 1. Enter the name of the plan you are enrolled in, from the front
cover of the plan brochure.
Item 2. Enter the present enrollment code from your plan or ID card.
Part C — FEHB Plan You Are Enrolling In or
Changing To.
Complete this part to enroll or change your enrollment in the FEHB.
Item 1. Enter the name of the plan you are enrolling in or changing
to. The plan name is on the front cover of the brochure of the
plan you want to be enrolled in.
Item 2. Enter the enrollment code of the plan you are enrolling in or
changing to. The enrollment code is on the front cover of the
brochure of the plan you want to be enrolled in, and shows
the plan and option you are electing and whether you are
enrolling for Self Only or Self and Family.
To enroll in a Health Maintenance Organization (HMO), you must live
(or in some cases work) in the geographic area specified by the carrier.
To enroll in an employee organization plan, you must be or become a
member of the plan’s sponsoring organization, as specified by the
carrier.
Your signature in Part F authorizes deductions from your annuity to
cover your cost of the enrollment you elect in this item, unless you are
required to make direct payments.
Part D — Event That Permits You to Enroll, Change
or Cancel.
Item 1. Enter the event code that permits you to enroll, change, or
cancel based on a Qualifying Life Event (QLE) from the
Table of Permissible Changes in Enrollment starting on page
5.
Explanation of Table of Permissible Changes in Enrollment
The tables on pages 5 through 8 illustrate when an annuitant, former
spouse, or person eligible for Temporary Continuation of Coverage
(TCC) may enroll or change enrollment. The tables show those
permissible events that are found in the FEHB regulations at 5 CFR
Part 890.
The tables have been organized by enrollee category. Each category is
designated by a number, which identifies the enrollee group, as follows:
2 Annuitants
3 Former spouses eligible for coverage under the Spouse Equity
provisions of FEHB law.
4 TCC enrollees.
Following each number is a letter which identifies a specific Qualifying
Life Event (QLE); for example, the event code 2A refers to open season.
Item 2. Enter the date of the QLE using numbers to show month, day,
and complete year; e.g., 06/30/2011. If you are electing to
enroll, enter the date you became eligible to enroll (for
example, the date your annuity was restored). If you are
making an open season enrollment or change, enter the date
on which the open season begins.
Part E — Suspension/Cancellation.
Check a box only if you wish to suspend or cancel your FEHB
enrollment. Also enter your present enrollment code in Part B.
You may suspend your FEHB enrollment because you are enrolling in
one of the following programs:
•
A Medicare HMO or Medicare Advantage plan,
•
Medicaid or similar State-sponsored program of medical assistance
for the needy,
•
TRICARE (including Uniformed Services Family Health Plan or
TRICARE for Life),
•
Peace Corps, or
•
CHAMPVA
You can reenroll in the FEHB Program if your other coverage ends.
If your coverage ends involuntarily, you can reenroll 31 days before
through 60 days after loss of coverage. If you want to reenroll in the
FEHB Program for a reason other than an involuntary loss of coverage,
you may do so during the next open season.
You must submit documentation of eligibility for coverage under the
non-FEHB Program to the Office of Personnel Management.
Initial the last box only if you wish to cancel your FEHB enrollment.
Also enter your present enrollment code in Part B. Be sure to read the
information below in the paragraph titled “Annuitants Who Cancel
Their Enrollment.”
Annuitants Who Cancel Their Enrollment
Generally, you cannot reenroll as an annuitant unless you are
continuously covered as a family member under another person’s
enrollment in the FEHB Program during the period between your
cancellation and reenrollment. OPM can advise you on events that allow
eligible annuitants to reenroll. If you cancel your enrollment because you
are covered under another FEHB enrollment, you can reenroll from 31
days before through 60 days after you lose that coverage under the other
enrollment.
If you cancel your enrollment for any other reason, you cannot
reenroll, and you and any family members covered by your enrollment
are not entitled to a 31-day temporary extension of coverage or to
convert to an individual policy.
Former Spouses (Spouse Equity) Who Cancel Their Enrollment
Generally, if you cancel your enrollment in the FEHB Program, you
cannot reenroll as a former spouse. However, if you cancel the
enrollment because you become covered under FEHB as a new spouse,
your eligibility for FEHB coverage under the Spouse Equity provisions
continues. You may reenroll as a former spouse from 31 days before
through 60 days after you lose coverage under the other FEHB
enrollment.
OPM Form 2809
2
Revised December 2013

If you cancel your enrollment for any other reason, you cannot
If you are registering for someone else under a written authorization
reenroll, and you and any family members covered by your enrollment from that person to do so, sign your name in Part F and attach the written
are not entitled to a 31-day temporary extension of coverage or to
authorization.
convert to an individual policy.
If you are registering as the court-appointed guardian for a former
Part F — Signature.
spouse eligible for coverage under the Spouse Equity provisions or for
Your retirement system cannot process your request unless you complete
an individual eligible for TCC, sign your name in Part F and attach
this part.
evidence of your court-appointed guardianship.
General Information
Dual Enrollment
No person (enrollee or family member) is entitled to receive benefits
under more than one enrollment in the Federal Employees Health
Benefits (FEHB) Program. Normally, you are not eligible to enroll if
you are covered as an annuitant under your own enrollment and as a
family member under someone else’s enrollment in the FEHB Program.
However, such dual enrollments may be permitted under certain
circumstances in order to:
•
Protect the interests of children who otherwise would lose coverage
as family members, or
•
Enable an employee who is under age 26 and covered under a
parent’s enrollment and who becomes the parent of a child to
enroll for Self and Family coverage.
(Each enrollee must notify his or her plan of the names of the persons to
be covered under his or her enrollment who are not covered under the
other enrollment.)
Enrollment in an HMO (Prepaid) Plan
To enroll in an HMO plan, you must live in the plan’s enrollment area as
stated in the plan brochure.
Enrollment in a Fee-for-Service Plan
If you enroll in a fee-for-service plan sponsored by an employee
organization, you must be (or become) a member of the organization that
sponsors the plan. Your membership will be verified.
Self Only Enrollment
A Self Only enrollment provides benefits just for you.
Self and Family Enrollment
A Self and Family enrollment provides benefits for you and your family
as described on page 1.
If your present enrollment is Self Only, you must change to a Self and
Family enrollment if you want to provide coverage for a new eligible
family member. See the table starting on page 5 for events which allow
you to change to a Self and Family enrollment.
Changes in Enrollment
After the Office of Personnel Management (OPM) processes your
request to enroll or change your enrollment, OPM will send you written
confirmation. Your health plan will mail a new identification (I.D.) card
to you as soon as possible. (OPM does not issue I.D. cards.) If you
should need health services before you receive your new I.D. card, show
the written confirmation you receive from OPM to the doctor or hospital.
They can then verify your new coverage with the plan.
Suspension or Cancellation of Enrollment
You may suspend or cancel your enrollment at any time for one of
several reasons.
If you cancel your enrollment because you are going to be continuously
covered as a family member under another person’s FEHB enrollment
during the period between your cancellation and reenrollment, you will
be eligible to reenroll when you lose coverage under that family
member’s enrollment.
If you suspend your FEHB Program enrollment to be covered by
a Medicare Advantage plan, Medicaid or a similar State-sponsored
program of medical assistance for the needy, TRICARE (including
Uniformed Services Family Health Plan or TRICARE for Life), Peace
Corps, or CHAMPVA, you will be eligible to enroll in the FEHB
Program if any of the above coverage ends.
Reenrollment Eligibility
If you cancel or suspend your enrollment as described above, you may
voluntarily reenroll in the FEHB Program during an annual open season.
If you involuntarily lose your Medicare Advantage plan, Medicaid or a
similar State-sponsored plan, TRICARE, Peace Corps, or CHAMPVA
coverage, you can reenroll in the FEHB Program effective the day after
your coverage ends. Your request to reenroll must be received at OPM
within the period beginning 31 days before and ending 60 days after
your coverage ends. Otherwise, you must wait until open season to
reenroll.
If you cancel your FEHB enrollment for a reason other than your
becoming covered under another FEHB enrollment, you cannot later
reenroll, and you and any family members will not be entitled to a
temporary extension of coverage or conversion to individual coverage.
Effective Dates of Changes
1. Open Season changes for annuitants take effect January 1.
2. Non-Open Season changes (except cancellations) take effect the first
day of the month following the month in which the Office of
Personnel Management (OPM) receives your OPM Form 2809.
Note: A change from Self Only to Self and Family due to the birth
of a child or addition of a child as a new family member is effective
the first day of the month in which the child is born or becomes an
eligible family member.
3. Cancellations: Your cancellation will take effect the end of the
month in which OPM receives your completed OPM Form 2809.
OPM Form 2809
3
Revised December 2013

Future Changes in Your Status
When your home or mailing address changes, you need to notify the
Office of Personnel Management immediately. Call our toll-free
number 1-888-767-6738 (TTY: 1-855-887-4957). Or, write to the
Change-of-Address Section, P.O. Box 440, Boyers, PA 16017-0440. Be
sure to include your new address, your name, and your retirement claim
number. You also need to notify your health benefits plan. If the family
member(s) covered by your health benefits enrollment change, you must
inform your health benefits plan. You must notify the Office of
Personnel Management immediately if you become the only person
covered by a Self and Family enrollment so that your enrollment can
be changed to Self Only. You must also inform the Office of Personnel
Management if you change your name or add family members.
For more information call our toll-free number 1-888-767-6738,
write to us, visit our web site, or send email.
Mailing Address: Office of Personnel Management
Retirement Operations Center
P.O. Box 45
Boyers, PA 16017-0045
Website: www.opm.gov/retirement-services/
Email: [email protected]
Privacy Act and Public Burden Statements
The information you provide on this form is needed to document your enrollment in the Federal Employees Health Benefits (FEHB) Program
under Chapter 89, title 5, U.S. Code. This information will be shared with the health insurance carrier you select so that it may (1) identify
your enrollment in the plan, (2) verify your and/or your family’s eligibility for payment of a claim for health benefits services or supplies, and
(3) coordinate payment of claims with other carriers with whom you might also make a claim for payment of benefits. This information may
be disclosed to other Federal agencies or Congressional offices which may have a need to know it in connection with your application for a
job, license, grant, or other benefit. It may also be shared and is subject to verification, via paper, electronic media, or through the use of
computer matching programs, with national, state, local, or other charitable or social security administrative agencies to determine and issue
benefits under their programs or to obtain information necessary for determination or continuation of benefits under this program. In addition,
to the extent this information indicates a possible violation of civil or criminal law, it may be shared and verified, as noted above, with an
appropriate Federal, state, or local law enforcement agency. While the law does not require you to supply all the information requested on this
form, doing so will assist in the prompt processing of your enrollment.
We request that you provide your Social Security Number so that it may be used as your individual identifier in the FEHB Program.
Executive Order 9397 (November 22, 1943) as amended by Executive Order 13478 (November 18, 2009), allows Federal agencies to use the
Social Security Number as an individual identifier to distinguish between people with the same or similar names. In addition, a mandatory
Insurer Reporting Law (Section 111 of Public Law No. 110-173) requires your health insurance carrier to report, as directed by the Secretary
of the Department of Health and Human Services (“Secretary”), information that the Secretary requires for purposes of coordination of
benefits between your health plan and Medicare. In order to properly coordinate Medicare payments with other insurance and/or workers’
compensation benefits, Medicare relies on your health insurance carrier to collect Medicare Claim Numbers or Social Security Numbers from
you and your eligible dependents. We therefore request that you provide a Medicare Claim Number or a Social Security Number for yourself
and each of your eligible dependents. Failure to furnish the requested information may result in the U.S. Office of Personnel Management’s
(OPM) inability to ensure the prompt payment of your and/or your family’s claims for health benefits services or supplies.
We estimate this form takes an average of 30 minutes to complete, including the time for reviewing instructions, getting the needed data, and
reviewing the completed form. Send comments regarding our time estimate or any other aspect of this form, including suggestions for
reducing completion time, to the Office of Personnel Management, Retirement Services Publications Team, (3206-0141), Washington, D.C.
20415-3430. The OMB number 3206-0141 is currently valid. OPM may not collect this information, and you are not required to respond,
unless this number is displayed.
OPM Form 2809
Revised December 2013
4
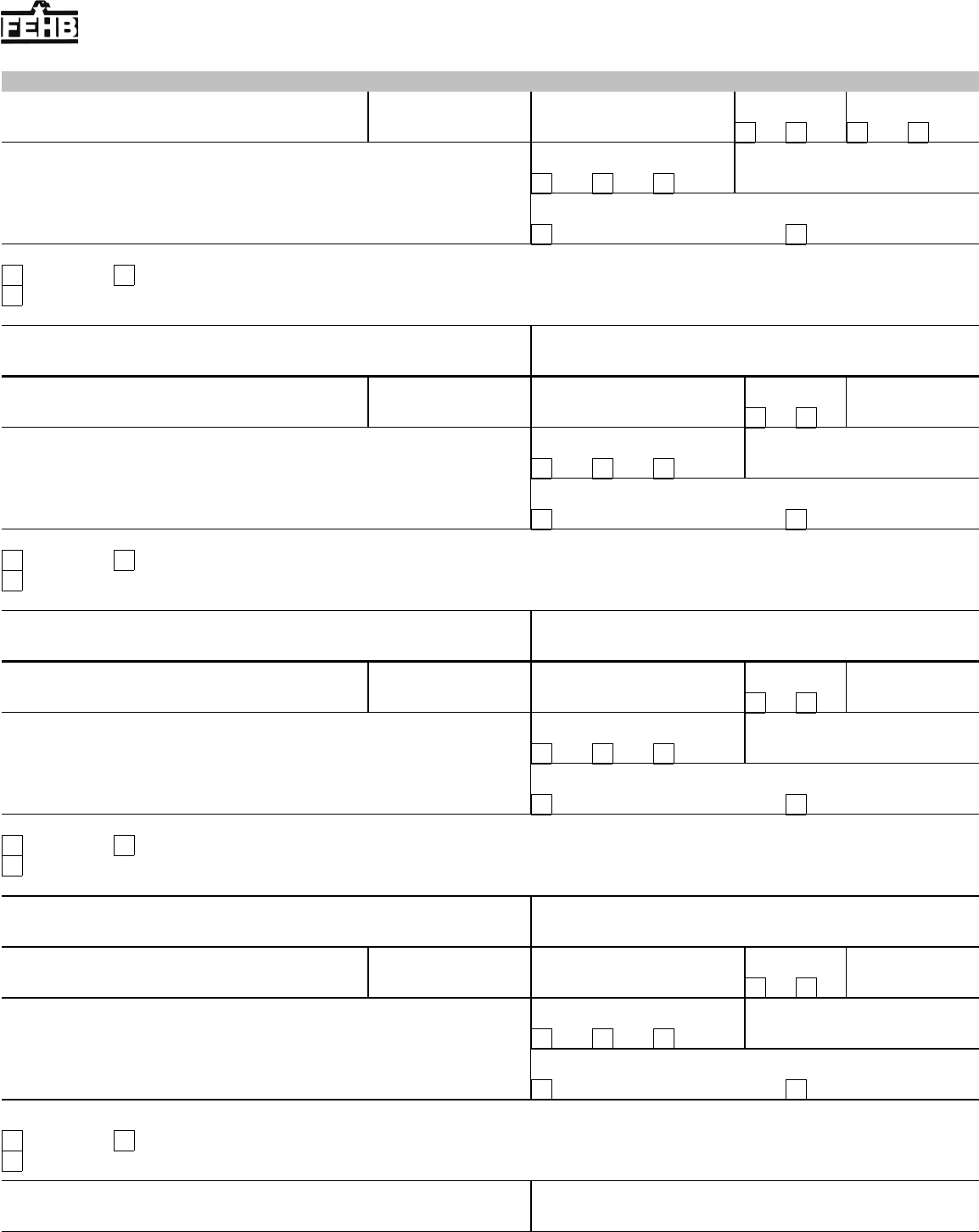
Tables of Permissible Changes in FEHB Enrollment
Enrollment May Be Cancelled or Changed From Family to Self Only at Any Time
QLE’s That Permit
Enrollment or Change
Change Permitted Time Limits
Event
Code
Event
From Not
Enrolled to
Enrolled
From Self
Only to Self
and Family
From One
Plan or
Option to
Another
When You Must File Health
Benefits Election Form With
the Office of Personnel
Management
2 Annuitant/Survivor Annuitant
Note for enrolled survivor annuitants: A change in family status based on additional family members can only occur if the additional
eligible family members are family members of the deceased employee or annuitant.
2A Open Season No Yes Yes As announced by OPM.
2B Change in family status; for example: marriage, birth or death
of family member, adoption, or divorce. Note: Survivors
cannot change plans because of the death of the annuitant.
No Yes Yes From 31 days before through 60
days after the event.
2C Reenrollment of annuitant who suspended FEHB enrollment
to enroll in a Medicare Advantage plan, Medicaid or similar
State-sponsored program, or to use TRICARE (including
Uniformed Services Family Health Plan and TRICARE for
Life), Peace Corps, or CHAMPVA, and who later
involuntarily loses this coverage under one of these
programs.
May reenroll N/A N/A From 31 days before through 60
days after involuntary loss of
coverage.
2D Reenrollment of annuitant who suspended FEHB enrollment
to enroll in a Medicare Advantage plan, Medicaid or similar
State-sponsored program, or to use TRICARE (including
Uniformed Services Family Health Plan or TRICARE for
Life), Peace Corps, or CHAMPVA, and who wants to reenroll
in the FEHB Program for any reason other than an involuntary
loss of coverage.
May reenroll N/A N/A During open season.
2E Restoration of annuity payments; for example:
•
Disability annuitant who was enrolled in FEHB, and whose
annuity terminated due to restoration of earning capacity or
recovery from disability, and whose annuity is restored;
•
Surviving spouse who was covered by FEHB immediately
before survivor annuity terminated because of remarriage
and whose annuity is restored;
•
Surviving child who was covered by FEHB immediately
before survivor annuity terminated because student status
ended and whose survivor annuity is restored;
•
Surviving child who was covered by FEHB immediately
before survivor annuity terminated because of marriage and
whose survivor annuity is restored.
Yes N/A N/A Within 60 days after the retirement
system mails a notice of insurance
eligibility.
2F Annuitant or eligible family member loses FEHB coverage
due to termination, cancellation, or change to Self Only of the
covering enrollment.
Yes Yes Yes From 31 days before through 60
days after date of loss of coverage.
2G Annuitant or eligible family member loses coverage under
another group insurance plan; for example:
•
Loss of coverage under another federally-sponsored health
benefits program;
Note: Annuitants who previously suspended FEHB to use a
Medicare Advantage Plan, TRICARE, Peace Corps, or
CHAMPVA, see codes 2C and 2D.
•
Loss of coverage under Medicaid or similar
State-sponsored program;
Note: Annuitants who previously suspended FEHB to use
Medicaid or a similar State-sponsored program, see codes
2C and 2D.
•
Loss of coverage due to termination of membership in the
employee organization sponsoring the FEHB plan;
•
Loss of coverage under a non-Federal health plan.
No Yes Yes From 31 days before through 60
days after loss of coverage.
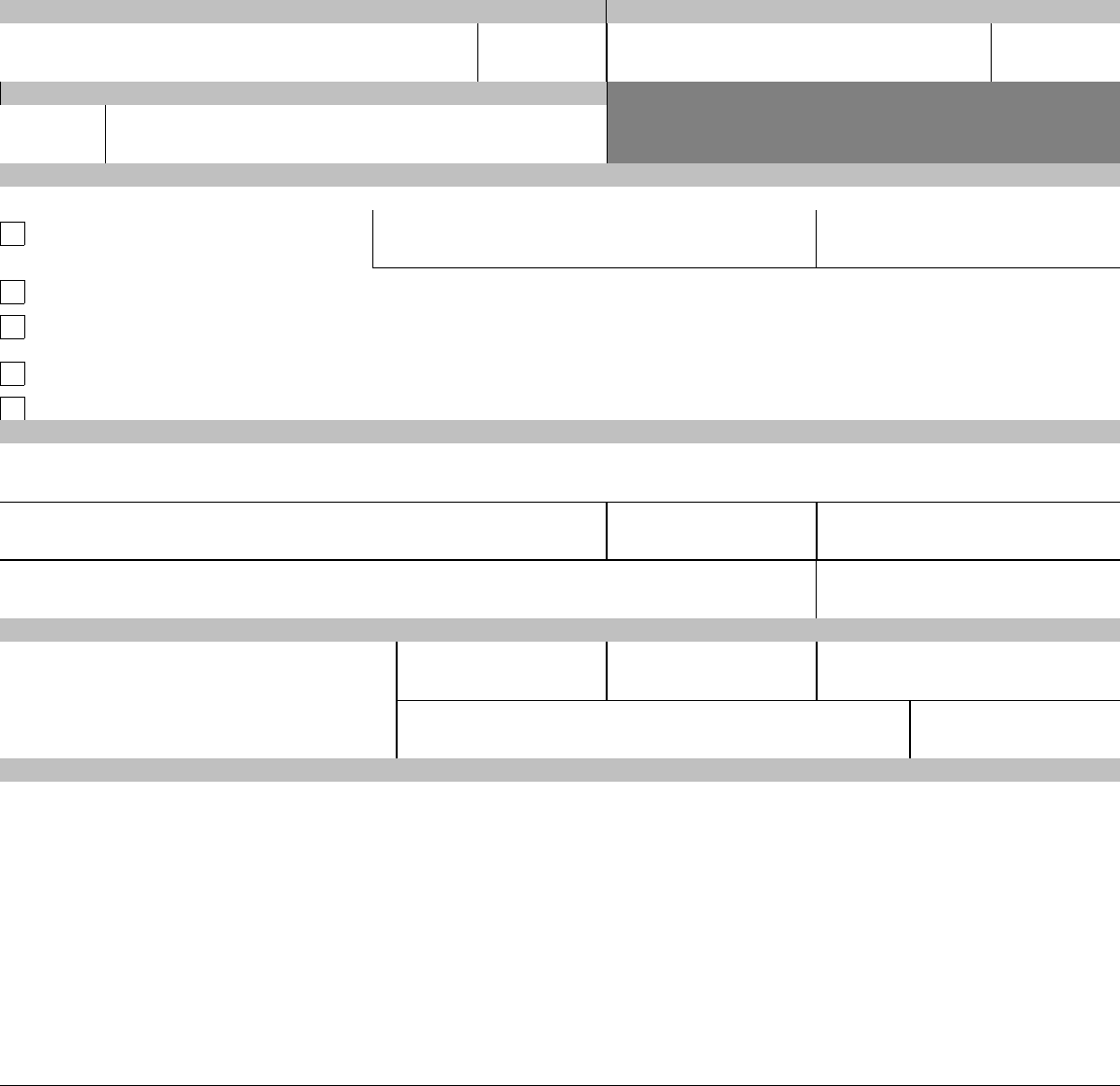
5
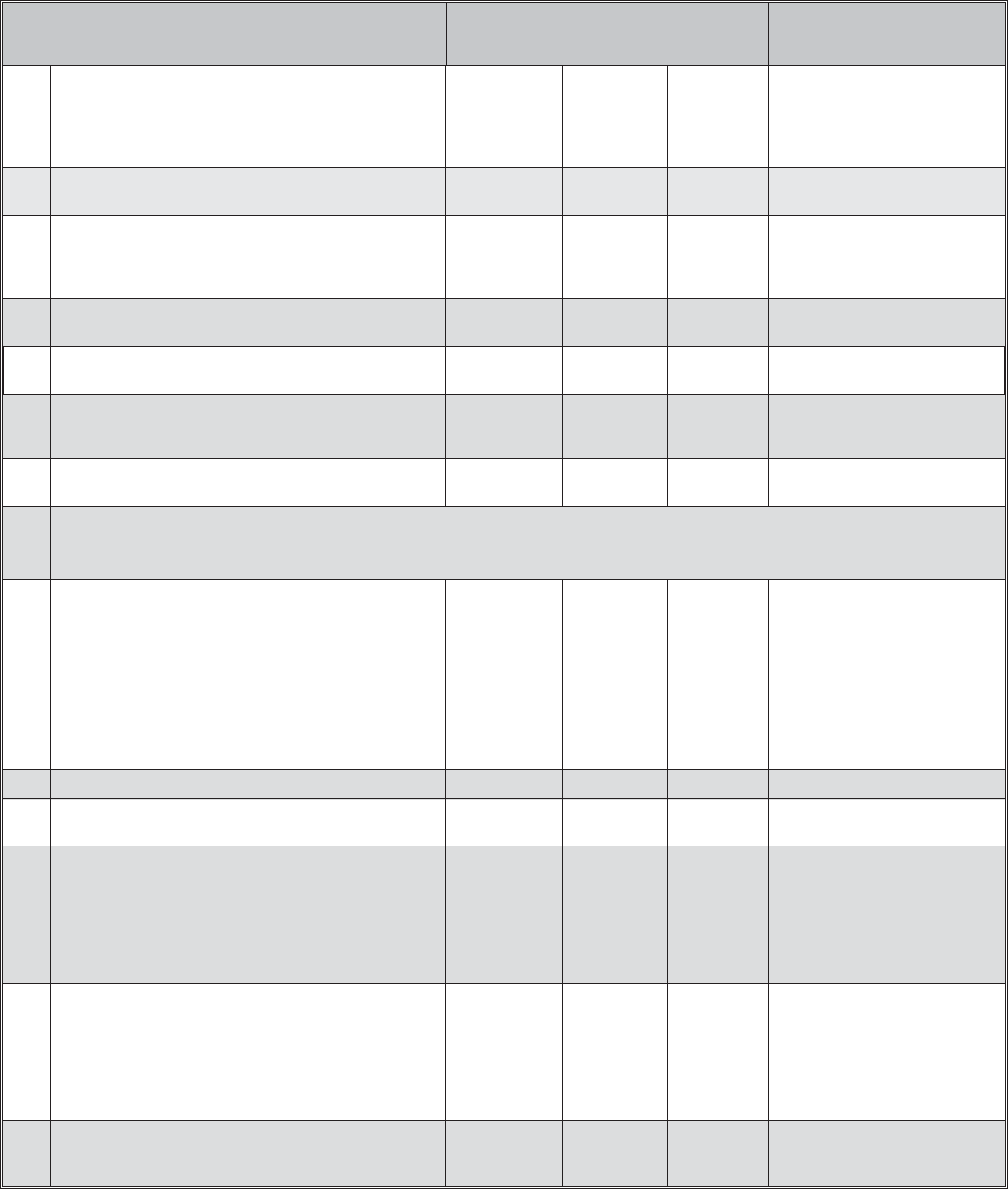
QLE’s That Permit
Enrollment or Change
Change Permitted Time Limits
Event
Code
Event
From Not
Enrolled to
Enrolled
From Self
Only to Self
and Family
From One
Plan or
Option to
Another
When You Must File Health
Benefits Election Form With
the Office of Personnel
Management
2H Annuitant or eligible family member loses coverage due to the
discontinuance, in whole or part, of an FEHB plan.
N/A Yes Yes During open season, unless OPM
sets a different time.
2I Annuitant or covered family member in a Health Maintenance
Organization (HMO) moves outside the geographic area from
which the carrier accepts enrollments, or if already outside this
area, moves further from this area.
N/A Yes Yes When you or a family member
notify OPM of a change of address
outside the plan’s service area.
2J Employee in an overseas post of duty retires or dies. No Yes Yes Within 60 days after retirement or
death.
2K An enrolled annuitant separates from duty after serving 31
days or more in a uniformed service.
N/A Yes Yes Within 60 days after separation
from the uniformed service.
2L On becoming eligible for Medicare.
(This change may be made only once in a lifetime.)
N/A No Yes At any time beginning on the 30th
day before becoming eligible for
Medicare.
2M Annuity is not sufficient to make withholdings for plan in
which enrolled.
N/A No Yes OPM will advise annuitant of the
options.
3 Former Spouse Under The Spouse Equity Provisions
Note: Former spouse may change to Self and Family only if family members are also eligible family members of the annuitant.
3A Initial opportunity to enroll. Former spouse must be eligible to
enroll under the authority of the Civil Service Retirement
Spouse Equity Act of 1984 (P.L. 98-615), as amended, the
Intelligence Authorization Act of 1986 (P.L. 99-569), or the
Foreign Relations Authorization Act, Fiscal Years 1988 and
1989 (P.L. 100-204).
Yes N/A N/A Generally, must apply within 60
days after dissolution of marriage.
However, if a retiring employee
elects to provide a former spouse
annuity or insurable interest annuity
for the former spouse, the former
spouse must apply within 60 days
after OPM’s notice of eligibility for
FEHB. May enroll any time after
OPM establishes eligibility.
3B Open Season. No Yes Yes As announced by OPM.
3C Change in family status based on addition of family members
who are also eligible family members of the annuitant.
No Yes Yes From 31 days before through 60
days after change in family status.
3D Reenrollment of former spouse who suspended FEHB
enrollment to enroll in a Medicare Advantage plan, Medicaid
or similar State-sponsored program, or to use TRICARE
(including Uniformed Services Family Health Plan or
TRICARE for Life), Peace Corps, or CHAMPVA, and who
later involuntarily loses this coverage under one of these
programs.
May reenroll N/A N/A From 31 days before through 60
days after involuntary loss of
coverage.
3E Reenrollment of former spouse who suspended FEHB
enrollment to enroll in a Medicare Advantage plan, Medicaid
or similar State-sponsored program, or to use TRICARE
(including Uniformed Services Family Health Plan or
TRICARE for Life), Peace Corps, or CHAMPVA, and who
wants to reenroll in the FEHB Program for any reason other
than an involuntary loss of coverage.
May reenroll N/A N/A During open season.
3F Former spouse or eligible child loses FEHB coverage due
to termination, cancellation, or change to Self Only of the
covering enrollment.
Yes Yes Yes From 31 days before through 60
days after date of loss of coverage.
6
QLE’s That Permit
Enrollment or Change
Change Permitted Time Limits
Event
Code
Event
From Not
Enrolled to
Enrolled
From Self
Only to Self
and Family
From One
Plan or
Option to
Another
When You Must File Health
Benefits Election Form With
the Office of Personnel
Management
3G Enrolled former spouse or eligible child loses coverage under
another group insurance plan; for example:
•
Loss of coverage under another federally-sponsored health
benefits program;
Note: Former spouses who previously suspended FEHB to
use a Medicare Advantage plan, TRICARE, Peace Corps,
or CHAMPVA, see codes 3D and 3E.
•
Loss of coverage under Medicaid or similar
State-sponsored program;
Note: Former spouses who previously suspended FEHB to
use Medicaid or a similar State-sponsored program, see
codes 3D and 3E.
•
Loss of coverage due to termination of membership in the
employee organization sponsoring the FEHB plan;
•
Loss of coverage under a non-Federal health plan.
N/A Yes Yes From 31 days before through 60
days after loss of coverage.
3H Former spouse or eligible family member loses coverage due
to the discontinuance, in whole or part, of an FEHB plan.
N/A Yes Yes During open season, unless OPM
sets a different time.
3I Former spouse or covered family member in a Health
Maintenance Organization (HMO) moves outside the
geographic area from which the carrier accepts enrollments,
or if already outside this area, moves further from this area.
N/A Yes Yes When you or a family member
notify OPM of a change of address
outside the plan’s service area.
3J On becoming eligible for Medicare
(This change may be made only once in a lifetime.)
N/A No Yes At any time beginning the 30th
day before becoming eligible for
Medicare.
3K Former spouse’s annuity is not sufficient to make FEHB
withholdings for plan in which enrolled.
No No Yes Retirement system will advise
former spouse of options.
4 Temporary Continuation of Coverage (TCC) For Eligible Former Spouses and Children.
Note: Former spouse may change to Self and Family only if family members are also eligible family members of the annuitant.
4A Opportunity to enroll for continued coverage under TCC
provisions:
•
Former spouse
•
Child who ceases to qualify as a family
member
Yes
Yes
N/A
N/A
N/A
N/A
Within 60 days after the qualifying
event, or receiving notice of
eligibility, whichever is later.
4B Open Season:
•
Former spouse
•
Child who ceases to qualify as a family
member
No
No
Yes
Yes
Yes
Yes
As announced by OPM.
4C Change in family status (except former spouse); for example,
marriage, birth or death of family member, adoption, or
divorce.
No Yes Yes From 31 days before through 60
days after event.
4D Change in family status of former spouse, based on addition
of family members who are eligible family members of the
employee or annuitant.
No Yes Yes From 31 days before through 60
days after event.
4E Reenrollment of a former spouse or child whose TCC
enrollment was terminated because of other FEHB coverage
and who loses the other FEHB coverage before the TCC
period of eligibility (18 or 36 months) expires.
May reenroll N/A N/A From 31 days before through 60
days after the event. Enrollment is
retroactive to the date of the loss of
the other FEHB coverage.
7
QLE’s That Permit
Enrollment or Change
Change Permitted Time Limits
Event
Code
Event
From Not
Enrolled to
Enrolled
From Self
Only to Self
and Family
From One
Plan or
Option to
Another
When You Must File Health
Benefits Election Form With
the Office of Personnel
Management
4F Enrollee or eligible family member loses coverage under
FEHB or another group insurance plan; for example:
•
Loss of coverage under another FEHB enrollment due to
termination, cancellation, or change to Self Only of the
covering enrollment (but see event 4E);
•
Loss of coverage under another federally-sponsored health
benefits program;
•
Loss of coverage due to termination of membership in the
employee organization sponsoring the FEHB plan;
•
Loss of coverage under Medicaid or similar
State-sponsored program;
•
Loss of coverage under a non-Federal health plan.
No Yes Yes From 31 days before through 60
days after loss of coverage.
4G Enrollee or eligible family member loses coverage due to the
discontinuance, in whole or part, of an FEHB plan.
N/A Yes Yes During open season, unless OPM
sets a different time.
4H Enrollee or covered family member in a Health Maintenance
Organization (HMO) moves outside the geographic area from
which the carrier accepts enrollments, or if already outside
this area, moves further from this area.
N/A Yes Yes When you or a family member
notify OPM of a change of address
outside the plan’s service area.
4I On becoming eligible for Medicare.
(This change may be made only once in a lifetime.)
N/A No Yes At any time beginning on the 30th
day before becoming eligible for
Medicare.
8
Form Approved:
Health Benefits Election Form
OMB No. 3206-0141
For Use By Annuitants and Former Spouses of Annuitants
Federal Employees
Health Benefits Program
8. Medicare Claim Number
7. If you are covered by Medicare,
check all that apply.
6. Mailing address (including ZIP Code)
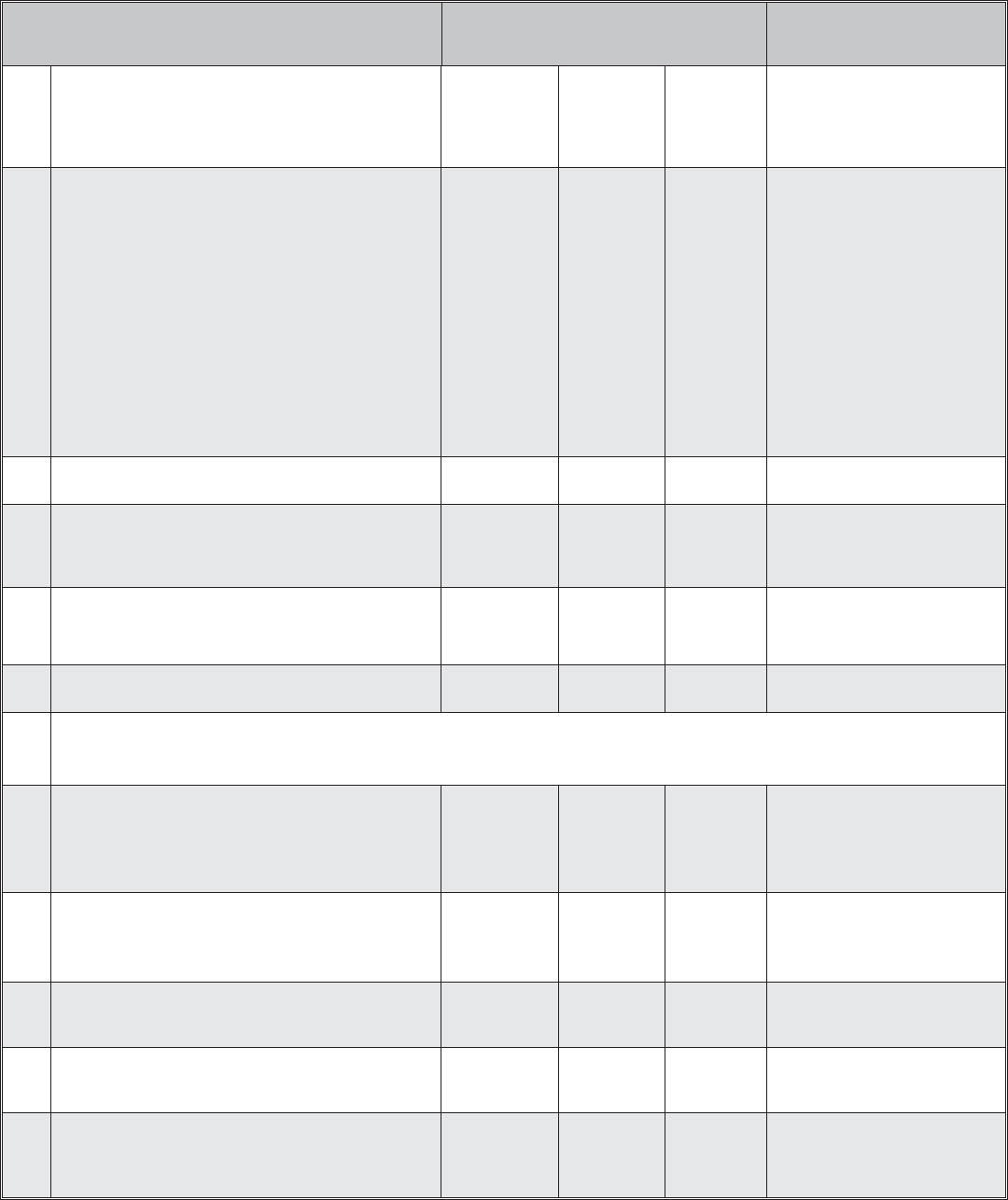
Part A - Enrollee and Family Member Information (for additional family members attach a separate sheet)
1. Enrollee name (last, first, middle initial) 2. Social Security Number 3. Date of birth (mm/dd/yyyy) 4. Sex
M F
5. Are you married?
Yes No
A B
_ _ / _ _ / _ _ _ _
D
9. Are you covered by insurance other than Medicare?
Yes, indicate in item 10 below. No
10. Indicate the type(s) of other insurance
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
TRICARE Other Name of other insurance: __________________________________________ Policy Number: _____________________
FEHB An FEHB self and family enrollment covers all eligible family members. No person may be covered under more than one FEHB enrollment. See instructions for
item 9 on page 1.
11. Email address 12. Preferred telephone number
_ _ / _ _ / _ _ _ _
13. Name of family member (last, first, middle initial) 14. Social Security Number 15. Date of birth (mm/dd/yyyy)
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
16. Sex 17. Relationship code
M F
19. If this family member is covered
18. Address (if different from enrollee) 20. Medicare Claim Number
by Medicare, check all that apply.
A B D
21. Is this family member covered by insurance other than Medicare?
Yes, indicate in item 22 below. No
22. Indicate the type(s) of other insurance
TRICARE Other Name of other insurance: ______________________________________________ Policy Number: _____________________
FEHB An FEHB self and family enrollment covers all eligible family members. No person may be covered under more than one FEHB enrollment. See instructions for
item 9 on page 1.
23. Email address (if applicable, enter email address of your spouse or adult child) 24. Preferred telephone number (if applicable, enter preferred phone number of
your spouse or adult child)
25. Name of family member (last, first, middle initial) 26. Social Security Number 27. Date of birth (mm/dd/yyyy)
_ _ / _ _ / _ _ _ _
28. Sex
M F
29. Relationship code
30. Address (if different from enrollee)
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
31. If this family member is covered
by Medicare, check all that apply.
A B D
32. Medicare Claim Number
33. Is this family member covered by insurance other than Medicare?
Yes, indicate in item 34 below. No
34. Indicate the type(s) of other insurance
TRICARE Other Name of other insurance: ______________________________________________ Policy Number: _____________________
FEHB An FEHB self and family enrollment covers all eligible family members. No person may be covered under more than one FEHB enrollment. See instructions for
item 9 on page 1.
35. Email address (if applicable, enter email address of your spouse or adult child)
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
36. Preferred telephone number (if applicable, enter preferred phone number of
your spouse or adult child)
_ _ / _ _ / _ _ _ _
37. Name of family member (last, first, middle initial) 38. Social Security Number 39. Date of birth (mm/dd/yyyy) 40. Sex 41. Relationship code
M F
43. If this family member is covered
42. Address (if different from enrollee) 44. Medicare Claim Number
by Medicare, check all that apply.
A B D
45. Is this family member covered by insurance other than Medicare?
Yes, indicate in item 46 below. No
46. Indicate the type(s) of other insurance
TRICARE Other Name of other insurance: ______________________________________________ Policy Number: _____________________
FEHB
An FEHB self and family enrollment covers all eligible family members. No person may be covered under more than one FEHB enrollment. See instructions for
item 9 on page 1.
47. Email address (if applicable, enter email address of your spouse or adult child) 48. Preferred telephone number (if applicable, enter preferred phone number of
your spouse or adult child)
Page 1 of 2
U.S. Office of Personnel Management OPM Form 2809
Previous edition is not usable. Revised December 2013
PRINT
Copy 1 - Enrollee
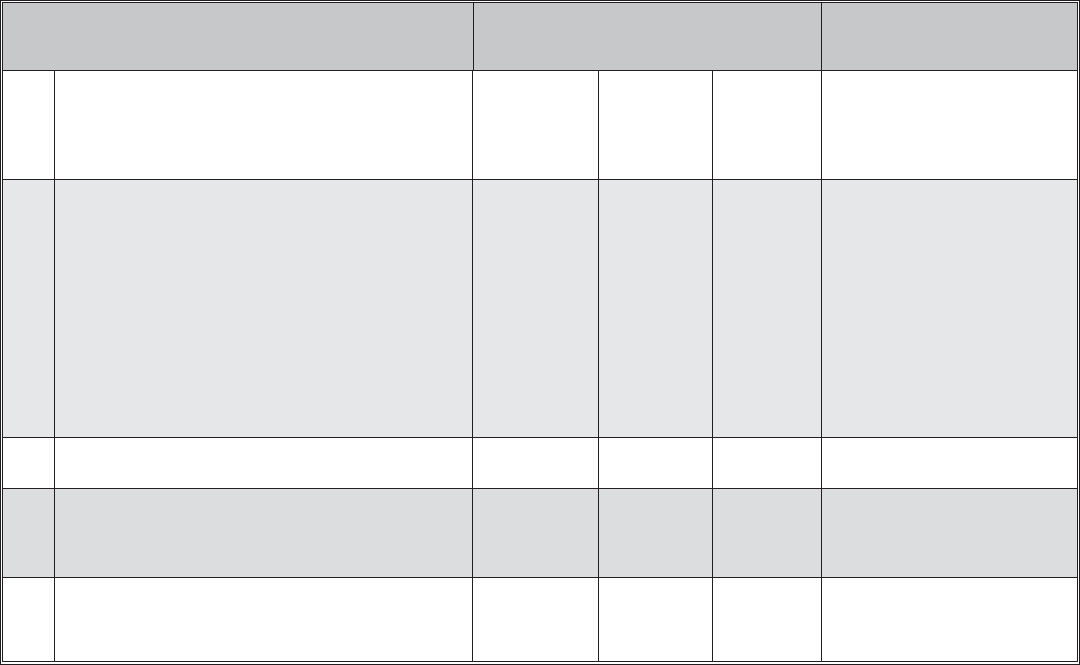
Part B - FEHB Plan You Are Currently Enrolled In (if applicable)
Part E - Election to Suspend/Cancel (fill in this part if you wish to suspend/cancel your enrollment in the FEHBP. See page 2 of the instructions.)
I elect to suspend or cancel my enrollment and have initialed the appropriate box below.
1. Plan name 2. Enrollment code
Part C - FEHB Plan You Are Enrolling In or Changing To
1. Plan name
2. Enrollment code
Part D - Event That Permits You To Enroll, Change, or Cancel (see page 2)
1. Event code 2. Date of event
_ _ / _ _ / _ _ _ _
Name
Social Security Number
I will be covered under the FEHB enrollment of:
I am covered by a Medicare Advantage plan, Medicaid or a similar State-sponsored program of medical assistance for the needy. I am enclosing evidence of my coverage.
I will be using CHAMPVA, TRICARE, or TRICARE for Life (enrollees over age 65 with Medicare Parts A and B). I am enclosing copies of my CHAMPVA authorization
card or my Uniformed Services identification card and, if over age 65, my Medicare card showing Parts A and B.
I am or will be covered by Peace Corps volunteer health benefits. I am enclosing evidence of my coverage.
Part F - Signature (all who register or cancel must fill in this part)
I am cancelling my enrollment for reasons other than the three situations shown above. I understand I can never reenroll in the FEHBP.
WARNING: Any intentionally false statement on this application or willful misrepresentation relative thereto is a violation of the law punishable by a fine of not more
than $10,000 or imprisonment of not more than 5 years, or both. (18 U.S.C. 1001.)
4. Payroll office number
6. Date
2. Date received in OPM 3. Effective date of action
5. Signature of authorized agency official
_ _ / _ _ / _ _ _ _ _ _ / _ _ / _ _ _ _
1. Your signature (do not print) 3. Retirement Claim Number 2. Date (mm/dd/yyyy)
_ _ / _ _ / _ _ _ _
Part G - To be Completed by OPM
1. Name and address
U.S. Office of Personnel Management
Retirement Services
Washington, D.C. 20415
24 90 0002
_ _ / _ _ / _ _ _ _
Remarks (For use by OPM only.)
5. Preferred telephone number 4. Email Address
Page 2 of 2
OPM Form 2809
Revised December 2013
PRINT
SAVE
CLEAR
Copy 1 - Enrollee



