Fillable Printable Infection Control Risk Assessment Template
Fillable Printable Infection Control Risk Assessment Template
Infection Control Risk Assessment Template
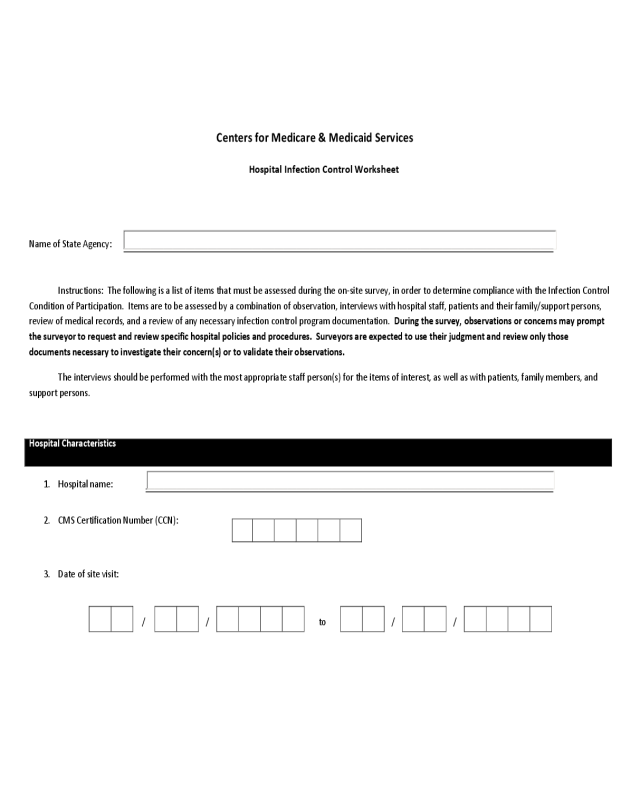
Centers for Medicare & Medicaid Services
Hospital Infection Control Worksheet
Name of State Agency: _________________________________________________________________________________________________
Instructions: The following is a list of items that must be assessed during the on-site survey, in order to determine compliance with the Infection Control
Condition of Participation. Items are to be assessed by a combination of observation, interviews with hospital staff, patients and their family/support persons,
review of medical records, and a review of any necessary infection control program documentation. During the survey, observations or concerns may prompt
the surveyor to request and review specific hospital policies and procedures. Surveyors are expected to use their judgment and review only those
documents necessary to investigate their concern(s) or to validate their observations.
The interviews should be performed with the most appropriate staff person(s) for the items of interest, as well as with patients, family members, and
support persons.
Hospital Characteristics
1. Hospital name: ____________________________________________________________________________________________
2. CMS Certification Number (CCN):
3. Date of site visit:
/ / to / /
2
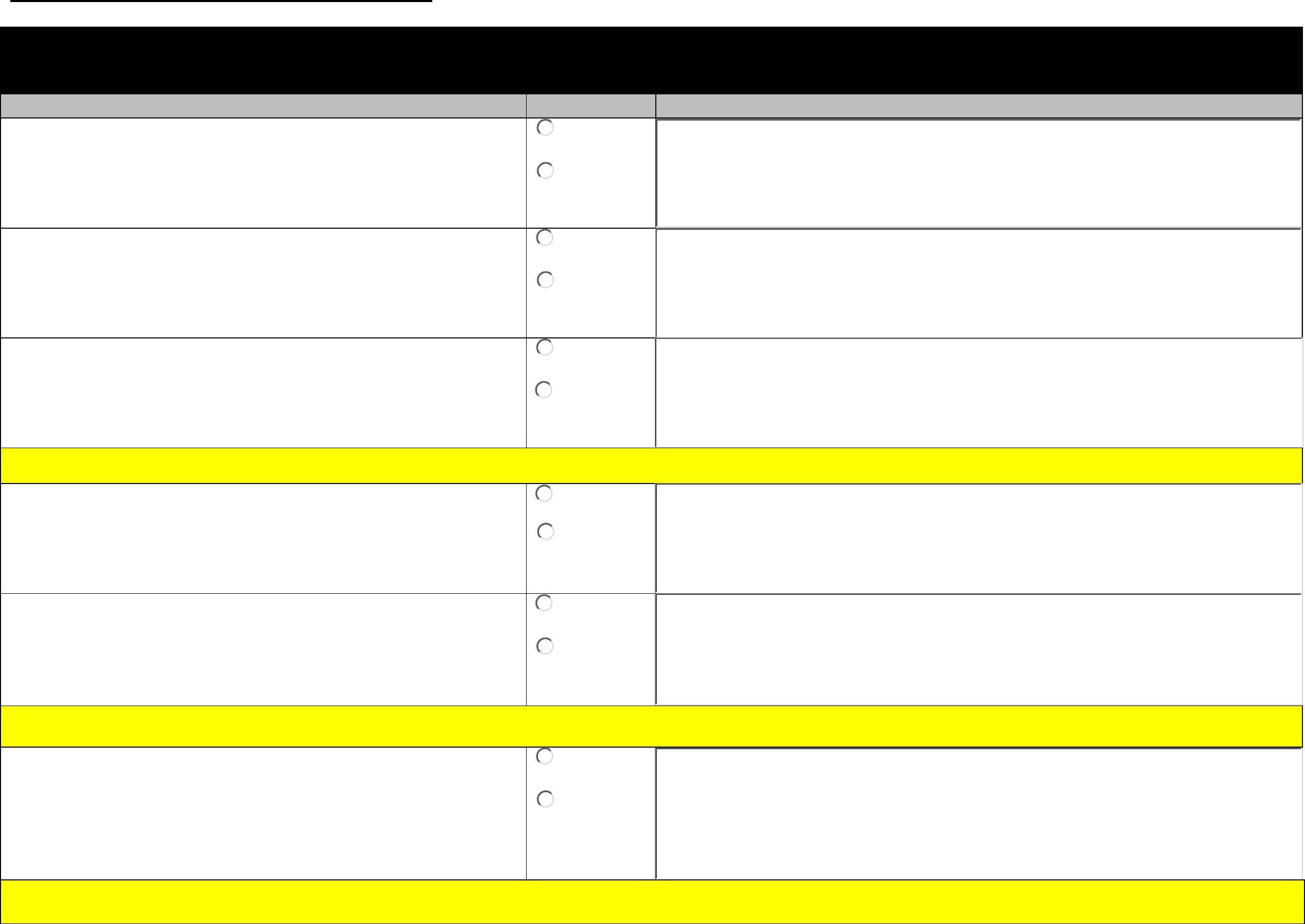
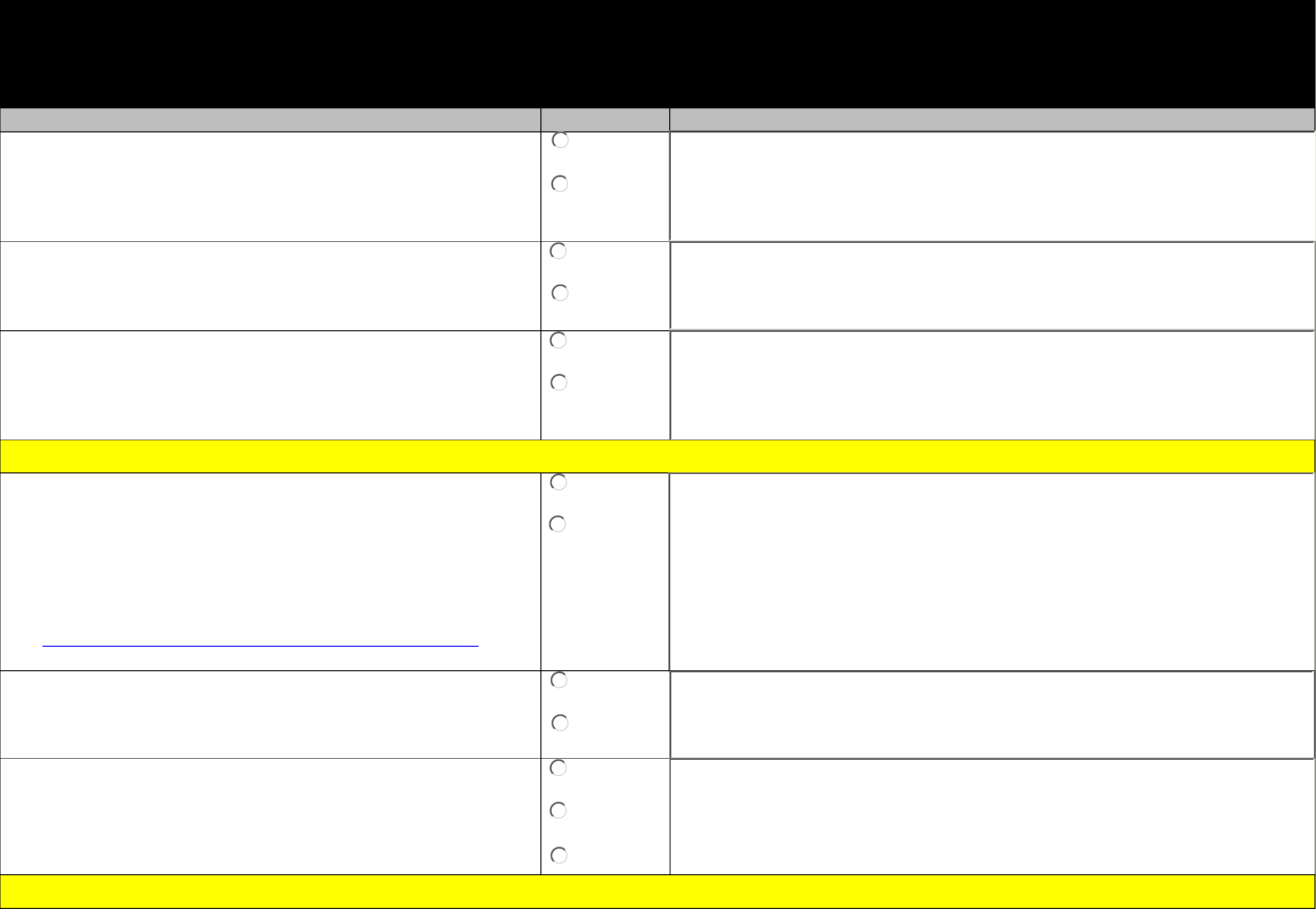
Module 1: Infection Prevention Program
Section 1.A. Infection Prevention Program and Resources
Elements to be assessed Surveyor Notes
1.A.1 The hospital has designated one or more individual(s) as its
Infection Control Officer(s).
¡
Yes
¡
No
1.A.2 The hospital has evidence that demonstrates the Infection
Control Officer(s) is qualified and maintain(s) qualifications
through education, training, experience or certification related
to infection control consistent with hospital policy.
¡
Yes
¡
No
1.A.3 The Infection Control Officer(s) can provide evidence that the
hospital has developed general infection control policies and
procedures that are based on nationally recognized guidelines
and applicable state and federal law.
¡
Yes
¡
No
If no to any of 1.A.1 through 1.A.3, cite at 42 CFR 482.42(a) (Tag A-748)
1.A.4 The Infection Control Officer can provide an updated list of
diseases reportable to the local and/or state public health
authorities.
¡
Yes
¡
No
1.A.5 The Infection Control Officer can provide evidence that
hospital complies with the reportable diseases requirements of
the local health authority.
¡
Yes
¡
No
No citation risk for questions 1.A.4 and 1.A.5
1.A.6 The hospital has infection control policies and procedures
relevant to construction, renovation, maintenance, demolition,
and repair, including the requirement for an infection control
risk assessment (ICRA) to define the scope of the project and
need for barrier measures before a project gets underway.
¡
Yes
¡
No
If no to 1.A.6,
cite at
42 CFR 482.42(a) (Tag A-748)
3
Section 1.B. Hospital QAPI Systems Related to Infection Prevention
Elements to be assessed Surveyor Notes
The hospital infection prevention program is coordinated into the hospital QAPI program as evidenced by:
1.B.1 The Infection Control Officer(s) can provide evidence that
problems identified in the infection control program are
addressed in the hospital QAPI program (i.e., development and
implementation of corrective interventions, and ongoing
evaluation of interventions implemented for both success and
sustainability).
¡
Yes
¡
No
If no to 1.B.1, cite at 42 CFR 482.21(e)(3) (Tag A-0286)
1.B.2 Hospital leadership, including the CEO, Medical Staff, and the
Director of Nursing Services ensures the hospital implements
successful corrective action plans in affected problem area(s).
¡
Yes
¡
No
If no to 1.B.2, cite at 42 CFR 482.42(b)(2) (Tag A-0756)
1.B.3 The hospital utilizes a risk assessment process to prioritize
selection of quality indicators for infection prevention and
control.
¡
Yes
¡
No
If no to 1.B.3,
cite at
42 CFR 482.21(a)(2) (Tag A-0267)
4
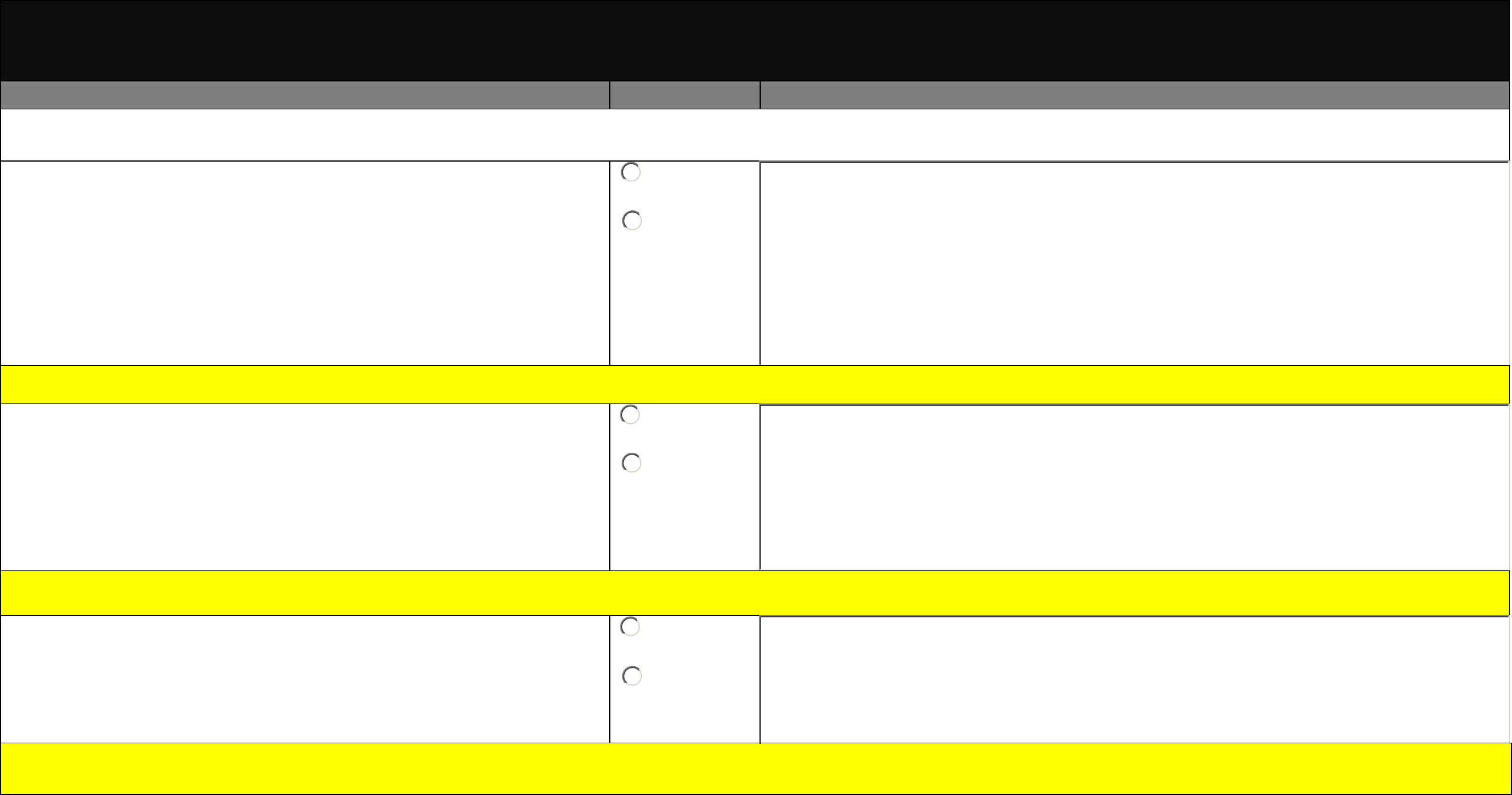
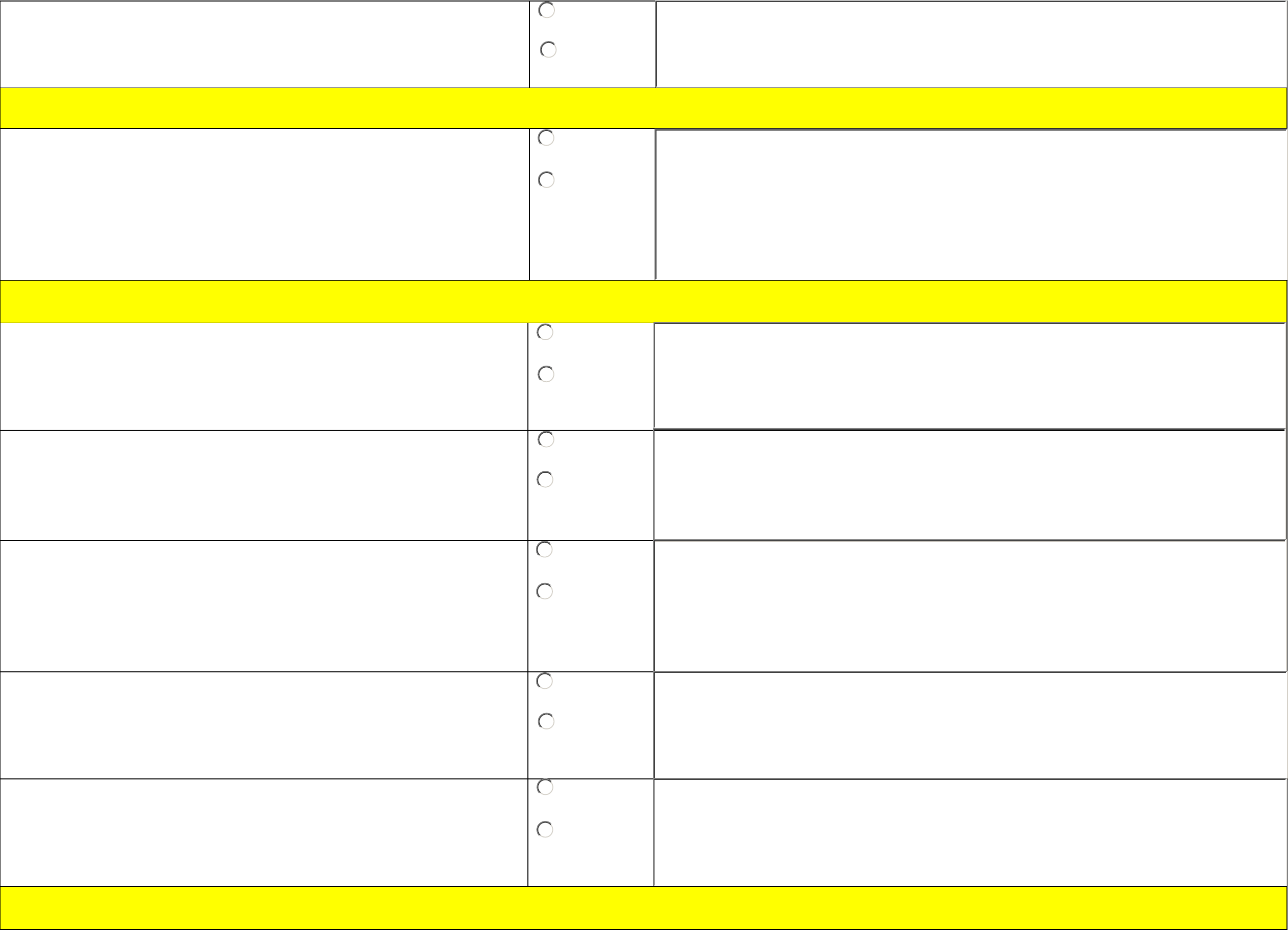
Section 1.C. Systems to Prevent Transmission of MDROs and Promote Antimicrobial
Stewardship
Elements to be assessed Surveyor Notes
1.C.1 The hospital has policies and procedures to minimize the risk of
development and transmission of multidrug-resistant organisms
(MDROs) within the hospital (applicable to all persons in the
hospital).
¡
Yes
¡
No
1.C.2
Systems are in place to designate patients known to be colonized
or infected with a targeted MDRO and to notify receiving units and
personnel prior to movement of such patients within the hospital.
¡
Yes
¡
No
1.C.3 Systems are in place to designate patients known to be colonized
or infected with a targeted MDRO and to notify receiving
healthcare facilities and personnel prior to transfer of such patient
between facilities.
¡
Yes
¡
No
If no to any part of 1.C.1 through 1.C.3, cite at 42 CFR 482.42(a) (Tag A-0749)
1.C.4 The hospital can provide a list of target MDROs.
Note: Hospitals should provide a list of MDROs that are targeted for
infection control because they are epidemiologically important
(e.g., MRSA, VRE). Please refer to CDC’s Guideline for Isolation
Precautions for criteria that may be used to define epidemiology
important organisms:
http://www.cdc.gov/hicpac/pdf/isolation/Isolation2007.pdf
¡
Yes
¡
No
1.C.5 The hospital can demonstrate the criteria used to determine
epidemiologically important MDROs on their list.
¡
Yes
¡
No
1.C.6 The hospital can provide justification for any epidemiologically
important organisms not on their list and otherwise not targeted
in their hospital.
¡
Yes
¡
No
¡
N/A
No citation risk for questions 1.C.4 through 1.C.6; for information only.
5
1.C.7 The hospital has an established system(s)
to ensure prompt
notification to the Infection Control Officer when a novel resistance
pattern based on microbiology results is detected.
¡
Yes
¡
No
If no to 1.C.7, cite at 42 CFR 482.42(a) (Tag A-0749)
1.C.8 Patients identified
as colonized or infected with target MDROs
are placed on Contact Precautions.
Note: This does not imply that hospitals are required to perform
active surveillance testing to detect MDRO colonization among a
specific subset or all patients.
¡
Yes
¡
No
If no to 1.C.8,
cite at
42 CFR 482.42(a) (Tag A-0749)
1.C.9 The hospital has written policies and procedures whose purpose
is to improve antibiotic use (antibiotic stewardship).
¡
Yes
¡
No
1.C.10 The hospital has designated a leader (e.g., physician,
pharmacist, etc.) responsible for program outcomes of antibiotic
stewardship activities at the hospital.
¡
Yes
¡
No
1.C.11 The hospital’s antibiotic stewardship policy and procedures
requires practitioners to document in the medical record or during
order entry an indication for all antibiotics, in addition to other
required elements such as does and duration.
¡
Yes
¡
No
1.C.12 The hospital has a formal procedure for all practitioners to
review the appropriateness of any antibiotics prescribed after 48
hours from the initial orders (e.g., antibiotic time out).
¡
Yes
¡
No
1.C.13 The hospital monitors antibiotic use (consumption) at the unit
and/or hospital level.
¡
Yes
¡
No
No citation risk for 1.C.9 through 1.C.13; for information only.
6
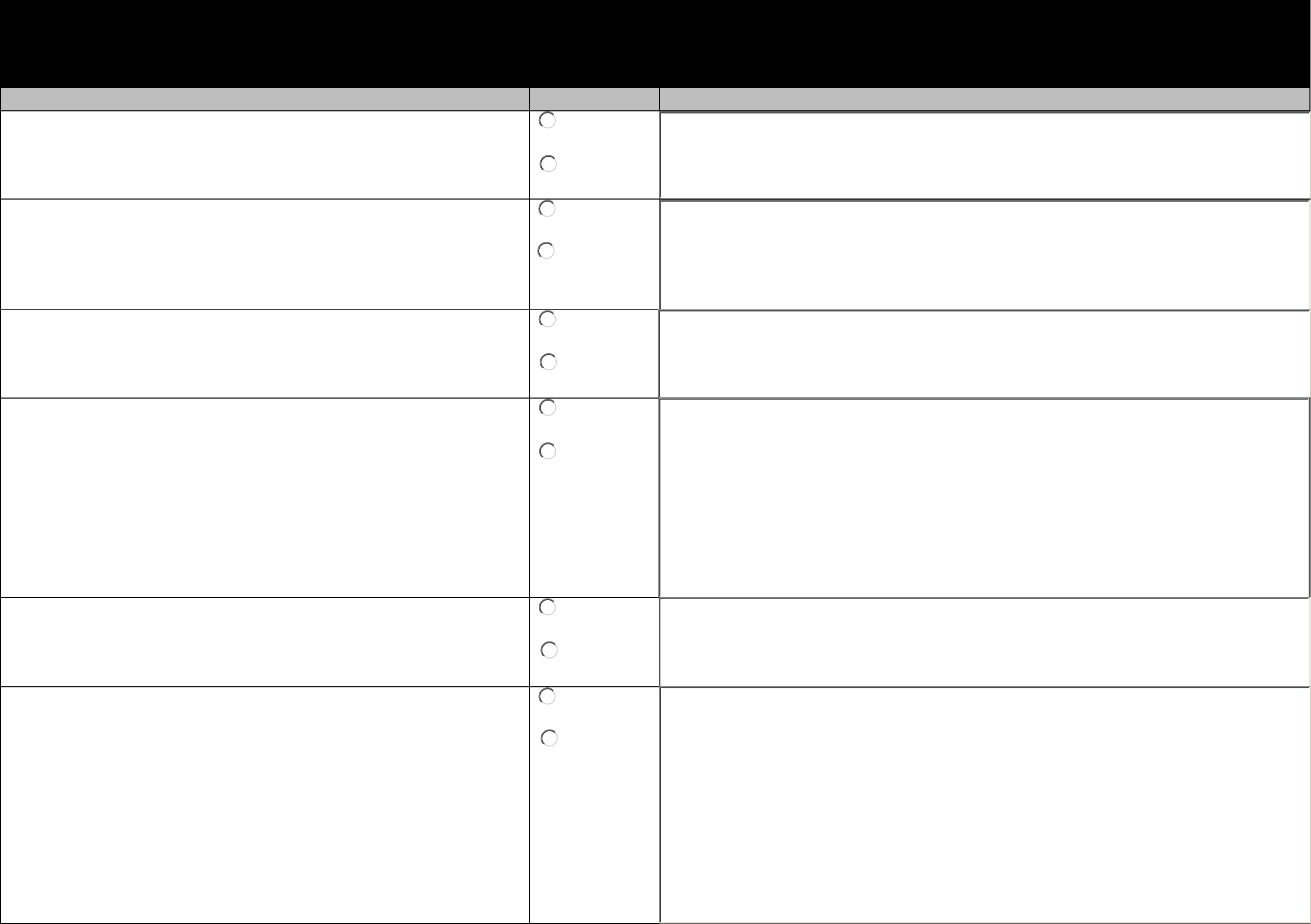
Section 1.D. Infection Prevention Systems, and Training Related to Personnel
Elements to be assessed Surveyor Notes
1.D.1 Personnel receive job-specific training on hospital infection
control practices, policies, and procedures upon hire and at
regular intervals.
¡
Yes
¡
No
1.D.2 The hospital infection control system trains personnel
expected to have contact with blood or other potentially
infectious material is anticipated on the blood borne pathogen
standards upon hire, at regular intervals, and as needed.
¡
Yes
¡
No
1.D.3 The hospital infection control system puts in place and
monitors efforts to prevent needle sticks, sharps injuries, and
other employee exposure events.
¡
Yes
¡
No
1.D.4 Following an exposure incident, post-exposure evaluation and
follow-up including prophylaxis as appropriate, is available to
the individual and performed by or under the supervision of a
practitioner.
Note: An exposure incident refers to a specific eye, mouth, other
mucous membrane, non-intact skin, or parenteral contact with
blood or other potentially infectious materials that result from
the performance of an individual’s duties.
¡
Yes
¡
No
1.D.5 The hospital tracks healthcare personnel exposure events,
evaluates event data, and develops corrective action plans to
reduce the incidence of such events.
¡
Yes
¡
No
1.D.6 The hospital infection control system ensures all
personnel are
screenedfor tuberculosis (TB) upon hire and, for those with
negative results, determine ongoing TB screening criteria based
upon facility/unit risk classification.
Note: Risk classification based on aggregated rates of TB test
conversions are periodically reviewed by the Infection Control
Officer to determine the need for modification to the screening
and TB control measures due to increases or decreases in
transmission.
¡
Yes
¡
No
7
1.D.7 The hospital infection control system ensures personnel with
TB test conversions are provided with appropriate follow-up
(e.g. evaluation and treatment, as needed).
¡
Yes
¡
No
1.D.8 The hospital infection control system ensures the hospital has
a respiratory protection program that details required worksite-
specific procedures and elements for required respirator use.
¡
Yes
¡
No
1.D.9 The hospital infection control system ensures that respiratory
fit testing is provided at regular intervals to personnel at risk.
¡
Yes
¡
No
1.D.10 Hospital has well-defined policies concerning contact of
personnel with patients when personnel have potentially
transmissible conditions.
•
The hospital provides education to personnel on need for
prompt reporting of illness to supervisor and/or
occupational health.
¡
Yes
¡
No
If no to any of 1.D.1 through 1.D.10, cite at 42 CFR 482.42(a) (Tag A-0749)
1.D.11 Personnel competency and compliance with job-specific
infection prevention policies and procedures are ensured
through routine training and when the Infection Control Officer
has identified problems requiring additional training.
¡
Yes
¡
No
If no to 1.D.11,
cite at
42 CFR 482.42(b) (Tag A-0756)
8
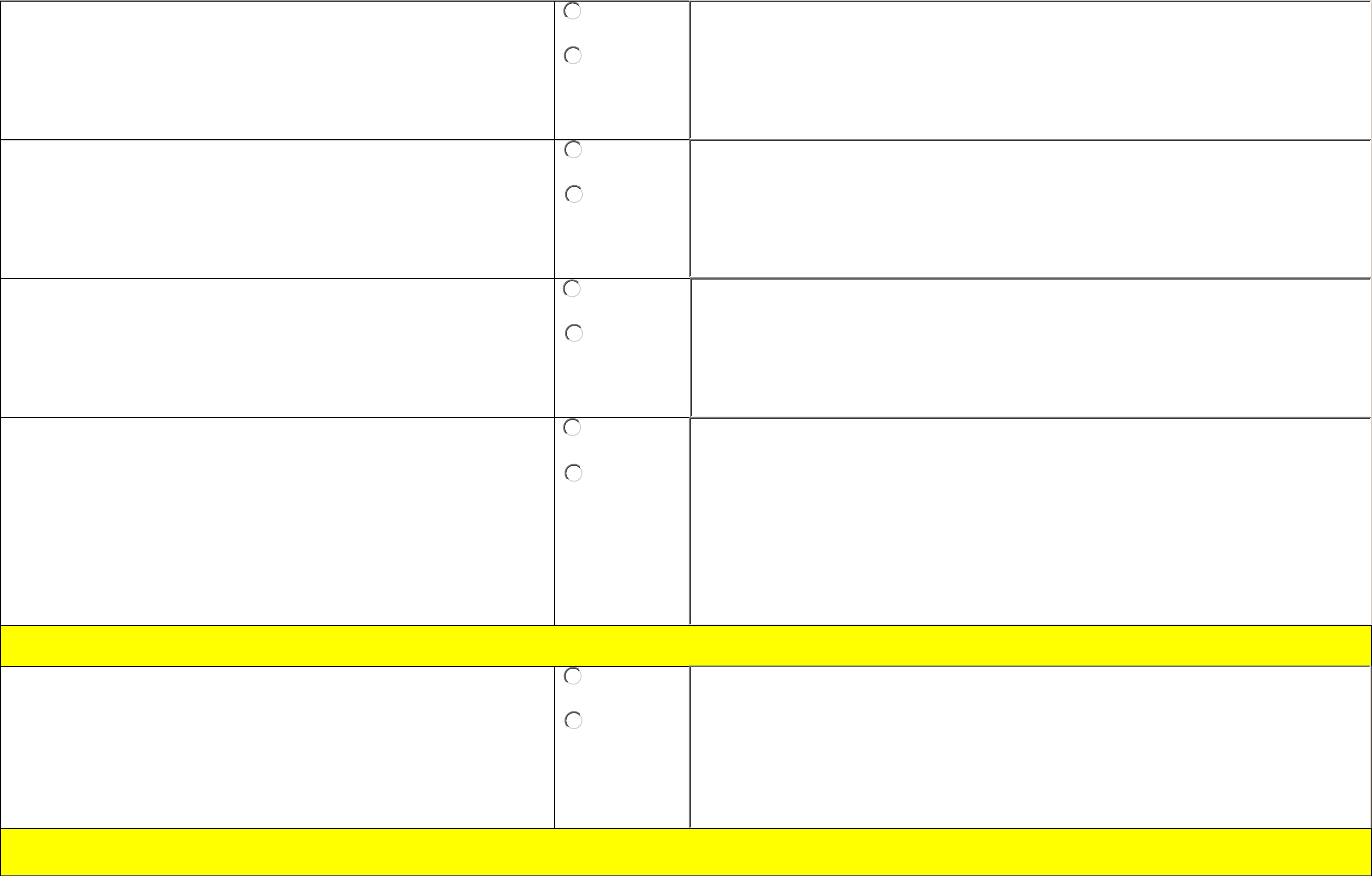
1.D.12 The hospital infection control system provides Hepatitis B
vaccination series to all employees who have potential
occupational exposure and offers post-vaccination testing for
immunity after the third vaccine dose is administered.
¡
Yes
¡
No
1.D.13 The hospital infection control system ensures and documents
that all personnel have presumptive evidence of immunity to
measles, mumps, and rubella.
¡
Yes
¡
No
1.D.14 The hospital infection control system provides Tdap (tetanus
toxoid, reduced diphtheria toxoid, and acellular pertussis)
vaccination for all personnel who have not previously received
Tdap.
Note:
Tdap is not licensed for multiple administrations; therefore,
after receipt of Tdap, HCP should receive Td (Tetanus diphtheria)
for future booster vaccination against tetanus and diphtheria.
¡
Yes
¡
No
1.D.15 The hospital infection control system ensures and documents
that all personnel have evidence of immunity to varicella.
¡
Yes
¡
No
1.D.16 The hospital infection control system ensures that all
personnel are offered annual influenza vaccination.
¡
Yes
¡
No
No citation risk for 1.D.12 through 1.D.16, for information only.
9
Module 2: General Infection Prevention Elements - to be applied to all locations providing patient care
Section 2.A. Hand Hygiene
Elements to be assessed Surveyor Notes
Hand hygiene is performed in a manner consistent with hospital infection control practices, policies, and procedures to maximize the prevention of infection and
communicable disease including the following:
Note: Observations for compliance with hand hygiene elements should be assessed throughout the hospital.
2.A.1 Soap, water, and a sink are readily accessible in appropriate
locations including, but not limited to, patient care areas and
food and medication preparation areas.
Note: Medications should not be prepared near areas of splashing
water (e.g. within 3 feet of a sink). Alternately when space is
limited, a splash guard can be mounted beside the sink.
¡
Yes
¡
No
2.A.2 Alcohol-based hand rub is readily accessible and placed in
appropriate locations. The locations may include:
•
Entrances to patient rooms,
•
At the bedside,
•
In individual pocket-sized containers carried by healthcare
personnel,
•
Staff workstations, and/or
•
Other convenient locations.
¡
Yes
¡
No
2.A.3 Personnel perform hand hygiene:
•
Before contact with the patient
•
Before performing an aseptic task (e.g., insertion of IV or
urinary catheter)
¡
Yes
¡
No
10
2.A.4 Personnel perform hand hygiene:
•
After contact with the patient
•
After contact with blood, body fluids, or visibly contaminated
surfaces
•
After removing gloves
¡
Yes
¡
No
2.A.5 Personnel perform hand hygiene using soap and water when
hands are visibly soiled (e.g., blood, body fluids) or after caring
for a patient with known or suspected C. difficile or norovirus
during an outbreak.
Note: In all other situations, alcohol-based hand rub is preferred.
¡
Yes
¡
No
2.A.6 Personnel do not wear artificial fingernails and/or extenders
when having direct contact with patients at high risk of
infection (e.g., those in intensive care units or ORs) per hospital
policy.
¡
Yes
¡
No
If no to any of 2.A.1 through 2.A.6, cite at 42 CFR 482.42(a) (Tag A-0749)
11
Section 2.B. Injection Practices and Sharps Safety (Medications and Infusates)
Elements to be assessed Surveyor Notes Surveyor Notes
Injections are given and sharps safety is managed in a manner consistent with hospital infection control policies and procedures to maximize the prevention of infection and
communicable disease including the following:
Note: If possible, questions in this section should be assessed through observation in two separate patient care areas or
settings of the hospital.
¡
Second observation not available (If selected,
questions 2.B.1 – 2.B.15 RIGHT column will be
blocked)
2.B.1 Injections are prepared using aseptic technique in an area
that has been cleaned and is free of contamination (e.g., visible
blood, or body fluids).
¡
Yes
¡
No
¡
Unable to
observe
¡
Yes
¡
No
¡
Unable to
observe
2.B.2 Needles are used for only one patient.
¡
Yes
¡
No
¡
Unable to
observe
¡
Yes
¡
No
¡
Unable to
observe
2.B.3 Syringes are used for only one patient (this includes
manufactured prefilled syringes).
¡
Yes
¡
No
¡
Unable to
observe
¡
Yes
¡
No
¡
Unable to
observe
2.B.4 Insulin pens are used for only one patient.
¡
Yes
¡
No
¡
Unable to
observe
¡
Yes
¡
No
¡
Unable to
observe
2.B.5 The rubber septum on all medication vials, whether
unopened or previously accessed, is disinfected with alcohol
prior to piercing.
¡
Yes
¡
No
¡
Unable to
observe
¡
Yes
¡
No
¡
Unable to
observe



