Fillable Printable Insurance Claim Sample Form
Fillable Printable Insurance Claim Sample Form
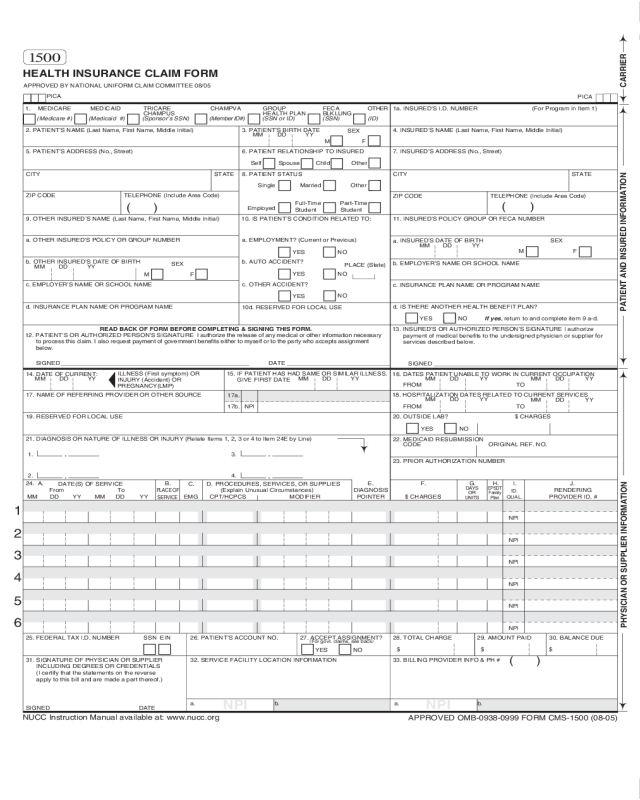
Insurance Claim Sample Form
1a. INSURED’S I.D. NUMBER
(For Program in Item 1)
4. INSURED’S NAME (Last Name, First Name, Middle Initial)
7. INSURED’S ADDRESS (No., Street)
CITY
STATE
ZIP CODE TELEPHONE (Include Area Code)
11. INSURED’S POLICY GROUP OR FECA NUMBER
a.
INSURED’S DATE OF BIRTH
b.
EMPLOYER’S NAME OR SCHOOL NAME
d. IS THERE ANOTHER HEALTH BENEFIT PLAN?
13. INSURED’S OR AUTHORIZED PERSON’S SIGNATURE I authorize
payment of medical benefits to the undersigned physician or supplier for
services described below.
SEX
F
HEALTH INSURANCE CLAIM FORM
OTHER
1. MEDICARE MEDICAID TRICARE CHAMPVA
READ BACK OF FORM BEFORE COMPLETING & SIGNING THIS FORM.
12. PATIENT’S OR AUTHORIZED PERSON’S SIGNATURE
I authorize the release of any medical or other information necessary
to process this claim. I also request payment of government benefits either to myself or to the party who accepts assignment
below.
SIGNED DATE
ILLNESS (First symptom) OR
INJURY (Accident) OR
PREGNANCY(LMP)
MM DD YY
15. IF PATIENT HAS HAD SAME OR SIMILAR ILLNESS.
GIVE FIRST DATE
MM DD YY
14. DATE OF CURRENT:
19. RESERVED FOR LOCAL USE
21. DIAGNOSIS OR NATURE OF ILLNESS OR INJURY (Relate Items 1, 2, 3 or 4 to Item 24E by Line)
From
MM DD YY
To
MM DD YY
1
2
3
4
5
6
25. FEDERAL TAX I.D. NUMBER SSN EIN 26. PATIENT’S ACCOUNT NO.
27. ACCEPT ASSIGNMENT?
(
For govt. claims, see back
)
31. SIGNATURE OF PHYSICIAN OR SUPPLIER
INCLUDING DEGREES OR CREDENTIALS
(I certify that the statements on the reverse
apply to this bill and are made a part thereof.)
SIGNED DATE
SIGNED
MM DD YY
FROM TO
FROM TO
MM DD YY
MM DD YY
MM DD YY
MM DD YY
CODE
ORIGINAL REF. NO.
$ CHARGES
28. TOTAL CHARGE 29. AMOUNT PAID 30. BALANCE DUE
$ $ $
PICA
PICA
2. PATIENT’S NAME (Last Name, First Name, Middle Initial)
5. PATIENT’S ADDRESS (No., Street)
CITY
STATE
ZIP CODE TELEPHONE
(Include Area Code)
9. OTHER INSURED’S NAME
(Last Name, First Name, Middle Initial)
a. OTHER INSURED’S POLICY OR GROUP NUMBER
b. OTHER INSURED’S DATE OF BIRTH
c. EMPLOYER’S NAME OR SCHOOL NAME
d.
INSURANCE PLAN NAME OR PROGRAM NAME
YES NO
( )
If yes
, return to and complete item 9 a-d.
16. DATES PATIENT UNABLE TO WORK IN CURRENT OCCUPATION
18. HOSPITALIZATION DATES RELATED TO CURRENT SERVICES
20. OUTSIDE LAB? $ CHARGES
22. MEDICAID RESUBMISSION
23. PRIOR AUTHORIZATION NUMBER
MM DD YY
CARRIER
PATIENT AND INSURED INFORMATION
PHYSICIAN OR SUPPLIER INFORMATION
M
F
YES NO
YES NO
1. 3.
2. 4.
DATE(S) OF SERVICE
PLACE OF
SERVICE
PROCEDURES, SERVICES, OR SUPPLIES
(Explain Unusual Circumstances)
CPT/HCPCS MODIFIER
DIAGNOSIS
POINTER
F
M
SEX
MM DD YY
YES
NO
YES
NO
YES
NO
PLACE (State)
GROUP
HEALTH PLAN
FECA
BLK LUNG
Single Married Other
3. PATIENT’S BIRTH DATE
6. PATIENT RELATIONSHIP TO INSURED
8. PATIENT STATUS
10. IS PATIENT’S CONDITION RELATED TO:
a.
EMPLOYMENT? (Current or Previous)
b. AUTO
ACCIDENT?
c. OTHER ACCIDENT?
10d. RESERVED FOR LOCAL USE
Employed
Student Student
Self Spouse
Child Other
(Medicare #) (Medicaid #) (Sponsor’s SSN) (Member ID#) (SSN or ID) (SSN) (ID)
( )
M
SEX
DAYS
OR
UNITS
F. H. I. J.24. A. B.
C. D.
E.
PROVIDER ID. #
17. NAME OF REFERRING PROVIDER OR OTHER SOURCE
17a.
EMG
RENDERING
32. SERVICE FACILITY LOCATION INFORMATION
33. BILLING PROVIDER INFO & PH #
NUCC Instruction Manual available at: www.nucc.org
c. INSURANCE PLAN NAME OR PROGRAM NAME
Full-Time Part-Time
17b. NPI
a. b. a. b.
NPI
NPI
NPI
NPI
NPI
NPI
APPROVED BY NATIONAL UNIFORM CLAIM COMMITTEE 08/05
G.
EPSDT
Family
Plan
ID.
QUAL.
NPI
NPI
CHAMPUS
( )
1500
APPROVED OMB-0938-0999 FORM CMS-1500 (08-05)
BECAUSE THIS FORM IS USED BY VARIOUS GOVERNMENT AND PRIVATE HEALTH PROGRAMS, SEE SEPARATE INSTRUCTIONS ISSUED BY
APPLICABLE PROGRAMS.
NOTICE: Any person who knowingly files a statement of claim containing any misrepresentation or any false, incomplete or misleading information may
be guilty of a criminal act punishable under law and may be subject to civil penalties.
REFERS TO GOVERNMENT PROGRAMS ONLY
MEDICARE AND CHAMPUS PAYMENTS: A patient’s signature requests that payment be made and authorizes release of any information necessary to process
the claim and certifies that the information provided in Blocks 1 through 12 is true, accurate and complete. In the case of a Medicare claim, the patient’s signature
authorizes any entity to release to Medicare medical and nonmedical information, including employment status, and whether the person has employer group health
insurance, liability, no-fault, worker’s compensation or other insurance which is responsible to pay for the services for which the Medicare claim is made. See 42
CFR 411.24(a). If item 9 is completed, the patient’s signature authorizes release of the information to the health plan or agency shown. In Medicare assigned or
CHAMPUS participation cases, the physician agrees to accept the charge determination of the Medicare carrier or CHAMPUS fiscal intermediary as the full charge,
and the patient is responsible only for the deductible, coinsurance and noncovered services. Coinsurance and the deductible are based upon the charge
determination of the Medicare carrier or CHAMPUS fiscal intermediary if this is less than the charge submitted. CHAMPUS is not a health insurance program but
makes payment for health benefits provided through certain affiliations with the Uniformed Services. Information on the patient’s sponsor should be provided in those
items captioned in “Insured”; i.e., items 1a, 4, 6, 7, 9, and 11.
BLACK LUNG AND FECA CLAIMS
The provider agrees to accept the amount paid by the Government as payment in full. See Black Lung and FECA instructions regarding required procedure and
diagnosis coding systems.
SIGNATURE OF PHYSICIAN OR SUPPLIER (MEDICARE, CHAMPUS, FECA AND BLACK LUNG)
I certify that the services shown on this form were medically indicated and necessary for the health of the patient and were personally furnished by me or were furnished
incident to my professional service by my employee under my immediate personal supervision, except as otherwise expressly permitted by Medicare or CHAMPUS
regulations.
For services to be considered as “incident” to a physician’s professional service, 1) they must be rendered under the physician’s immediate personal supervision
by his/her employee, 2) they must be an integral, although incidental part of a covered physician’s service, 3) they must be of kinds commonly furnished in physician’s
offices, and 4) the services of nonphysicians must be included on the physician’s bills.
For CHAMPUS claims, I further certify that I (or any employee) who rendered services am not an active duty member of the Uniformed Services or a civilian employee
of the United States Government or a contract employee of the United States Government, either civilian or military (refer to 5 USC 5536). For Black-Lung claims,
I further certify that the services performed were for a Black Lung-related disorder.
No Part B Medicare benefits may be paid unless this form is received as required by existing law and regulations (42 CFR 424.32).
NOTICE: Any one who misrepresents or falsifies essential information to receive payment from Federal funds requested by this form may upon conviction be subject
to fine and imprisonment under applicable Federal laws.
NOTICE TO PATIENT ABOUT THE COLLECTION AND USE OF MEDICARE, CHAMPUS, FECA, AND BLACK LUNG INFORMATION
(PRIVACY ACT STATEMENT)
We are authorized by CMS, CHAMPUS and OWCP to ask you for information needed in the administration of the Medicare, CHAMPUS, FECA, and Black Lung
programs. Authority to collect information is in section 205(a), 1862, 1872 and 1874 of the Social Security Act as amended, 42 CFR 411.24(a) and 424.5(a) (6), and
44 USC 3101;41 CFR 101 et seq and 10 USC 1079 and 1086; 5 USC 8101 et seq; and 30 USC 901 et seq; 38 USC 613; E.O. 9397.
The information we obtain to complete claims under these programs is used to identify you and to determine your eligibility. It is also used to decide if the services
and supplies you received are covered by these programs and to insure that proper payment is made.
The information may also be given to other providers of services, carriers, intermediaries, medical review boards, health plans, and other organizations or Federal
agencies, for the effective administration of Federal provisions that require other third parties payers to pay primary to Federal program, and as otherwise necessary
to administer these programs. For example, it may be necessary to disclose information about the benefits you have used to a hospital or doctor. Additional disclosures
are made through routine uses for information contained in systems of records.
FOR MEDICARE CLAIMS: See the notice modifying system No. 09-70-0501, titled, ‘Carrier Medicare Claims Record,’ published in the Federal Register, Vol. 55
No. 177, page 37549, Wed. Sept. 12, 1990, or as updated and republished.
FOR OWCP CLAIMS: Department of Labor, Privacy Act of 1974, “Republication of Notice of Systems of Records,” Federal Register Vol. 55 No. 40, Wed Feb. 28,
1990, See ESA-5, ESA-6, ESA-12, ESA-13, ESA-30, or as updated and republished.
FOR CHAMPUS CLAIMS: PRINCIPLE PURPOSE(S): To evaluate eligibility for medical care provided by civilian sources and to issue payment upon establishment
of eligibility and determination that the services/supplies received are authorized by law.
ROUTINE USE(S): Information from claims and related documents may be given to the Dept. of Veterans Affairs, the Dept. of Health and Human Services and/or
the Dept. of Transportation consistent with their statutory administrative responsibilities under CHAMPUS/CHAMPVA; to the Dept. of Justice for representation of
the Secretary of Defense in civil actions; to the Internal Revenue Service, private collection agencies, and consumer reporting agencies in connection with recoupment
claims; and to Congressional Offices in response to inquiries made at the request of the person to whom a record pertains. Appropriate disclosures may be made
to other federal, state, local, foreign government agencies, private business entities, and individual providers of care, on matters relating to entitlement, claims
adjudication, fraud, program abuse, utilization review, quality assurance, peer review, program integrity, third-party liability, coordination of benefits, and civil and
criminal litigation related to the operation of CHAMPUS.
DISCLOSURES: Voluntary; however, failure to provide information will result in delay in payment or may result in denial of claim. With the one exception discussed
below, there are no penalties under these programs for refusing to supply information. However, failure to furnish information regarding the medical services rendered
or the amount charged would prevent payment of claims under these programs. Failure to furnish any other information, such as name or claim number, would delay
payment of the claim. Failure to provide medical information under FECA could be deemed an obstruction.
It is mandatory that you tell us if you know that another party is responsible for paying for your treatment. Section 1128B of the Social Security Act and 31 USC 3801-
3812 provide penalties for withholding this information.
You should be aware that P.L. 100-503, the “Computer Matching and Privacy Protection Act of 1988”, permits the government to verify information by way of computer matches.
MEDICAID PAYMENTS (PROVIDER CERTIFICATION)
I hereby agree to keep such records as are necessary to disclose fully the extent of services provided to individuals under the State’s Title XIX plan and to furnish
information regarding any payments claimed for providing such services as the State Agency or Dept. of Health and Human Services may request.
I further agree to accept, as payment in full, the amount paid by the Medicaid program for those claims submitted for payment under that program, with the exception
of authorized deductible, coinsurance, co-payment or similar cost-sharing charge.
SIGNATURE OF PHYSICIAN (OR SUPPLIER): I certify that the services listed above were medically indicated and necessary to the health of this patient and were
personally furnished by me or my employee under my personal direction.
NOTICE: This is to certify that the foregoing information is true, accurate and complete. I understand that payment and satisfaction of this claim will be from Federal and State
funds, and that any false claims, statements, or documents, or concealment of a material fact, may be prosecuted under applicable Federal or State laws.
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB
control number for this information collection is 0938-0999. The time required to complete this information collection is estimated to average 10 minutes per response, including the
time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. If you have any comments concerning the
accuracy of the time estimate(s) or suggestions for improving this form, please write to: CMS, Attn: PRA Reports Clearance Officer, 7500 Security Boulevard, Baltimore, Maryland
21244-1850.
This address is for comments and/or suggestions only. DO NOT MAIL COMPLETED CLAIM FORMS TO THIS ADDRESS.
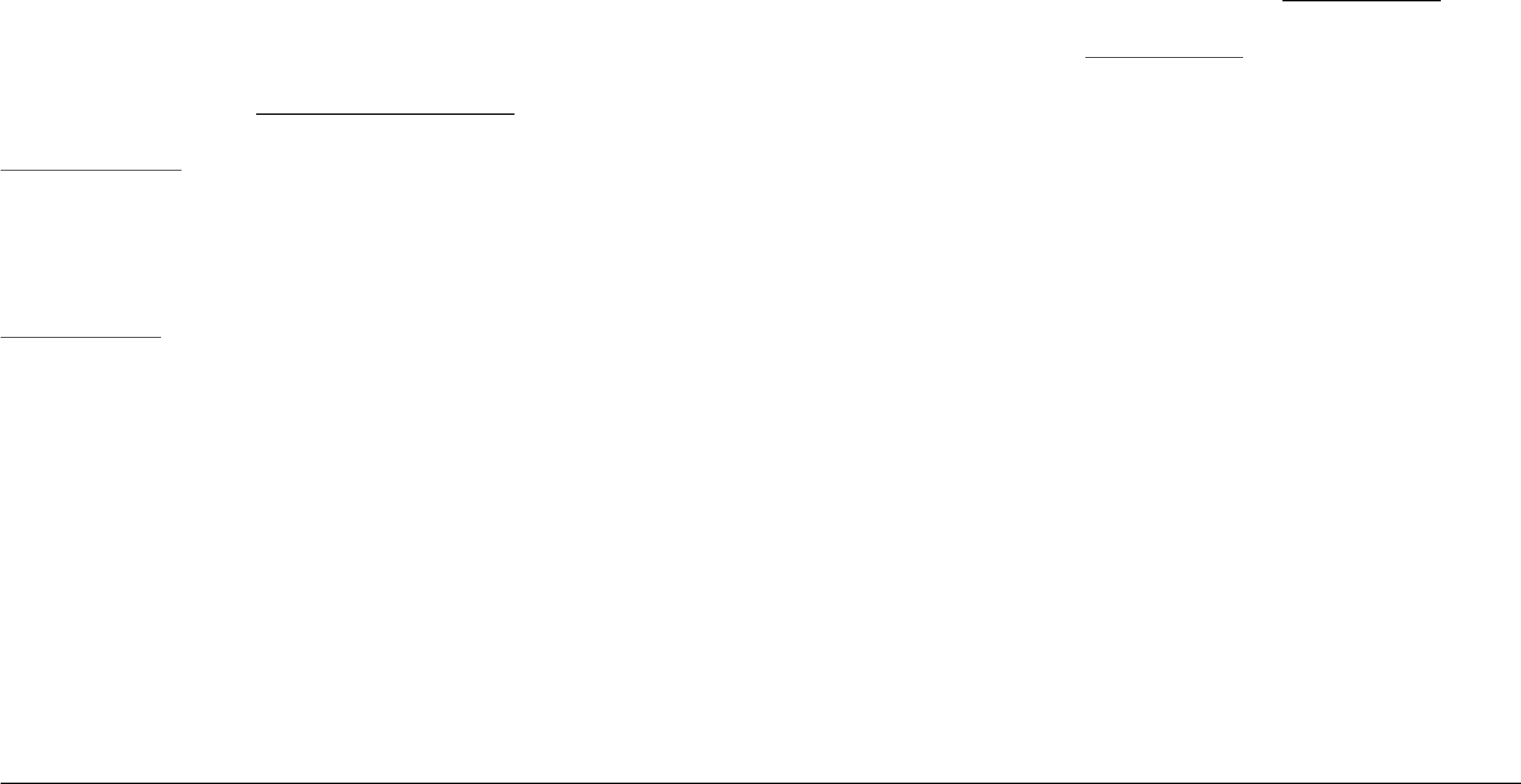
__ __ __
1 2
4 TYPE
OF BILL
FROM THROUGH
5 FED.TAX NO.
a
b
c
d
DX
ECI
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
A
B
C
A B C D E F G
H
I J K L
M
N O P Q
a
b
c
a
b
c
a
b
c
d
ADMISSION
CONDITION CODES
DATE
OCCURRENCE OCCURRENCE OCCURRENCE OCCURRENCE SPAN OCCURRENCE SPAN
CODEDATE CODE CODE CODE DATE
CODE THROUGH
VALUE CODES VALUE CODES VALUE CODES
CODE AMOUNT
CODE AMOUNT
CODEAMOUNT
TOTALS
PRINCIPAL PROCEDURE a. OTHER PROCEDURE b.OTHER PROCEDURE
NPI
CODE DATE CODE DATE CODE DATE
FIRST
c. d. e.OTHER PROCEDURE
NPI
CODE DATE DATE
FIRST
NPI
b
LAST
FIRST
c
NPI
d
LAST
FIRST
UB-04 CMS-1450
7
10 BIRTHDATE 11 SEX
12 13 HR 14 TYPE
15 SRC
DATE
16
DHR
181920
FROM
21 2522 26 2823 27
CODE FROM
DATE
OTHER
PRV ID
THE CERTIFICATIONS ON THE REVERSE APPLY TO THIS BILL AND ARE MADE A PART HEREOF.
b
.
INFO
BEN.
CODE
OTHER PROCEDURE
THROUGH
29
ACDT
30
3231 33 34 35 36 37
38 39 40 41
42 REV.CD. 43 DESCRIPTION 45 SERV.DATE 46 SERV.UNITS 47 TOTAL CHARGES 48 NON-COVERED CHARGES 49
52REL
51 HEALTH PLAN ID
53ASG.
54 PRIOR PAYMENTS
55 EST.AMOUNT DUE
56 NPI
57
58
INSURED’S
NAME 59
P.REL 60
INSURED’S
UNIQUE
ID
61
GROUP
NAME
62
INSURANCE
GROUP
NO.
64 DOCUMENT CONTROL NUMBER
65 EMPLOYER NAME
66
67
68
69 ADMIT 70 PATIENT
72
73
74
75
76
ATTENDING
80
REMARKS
OTHER PROCEDURE
a
77
OPERATING
78
OTHER
79
OTHER
81CC
CREATION DATE
3a
PAT.
CNTL
#
24
b.MED.
REC. #
44 HCPCS / RATE / HIPPS CODE
PAGE OF
APPROVED OMB NO. 0938-0997
e
a
8 PATIENT NAME
50 PAYER NAME
63 TREATMENT AUTHORIZATION CODES
6
STATEMENT
COVERS
PERIOD
9 PATIENT ADDRESS
17
STAT
STATE
DX
REASON DX
71 PPS
CODE
QUAL
LAST
LAST
National Uniform
Billing Committee
NUBC
™
OCCURRENCE
QUAL
QUAL
QUAL
CODE DATE
A
B
C
A
B
C
A
B
C
A
B
C
A
B
C
a
b
a
b

Submission of this claim constitutes certification that the billing
information as shown on the face hereof is true, accurate and complete.
That the submitter did not knowingly or recklessly disregard or
misrepresent or conceal material facts. The following certifications or
verifications apply where pertinent to this Bill:
1. If third party benefits are indicated, the appropriate assignments by
the insured /beneficiary and signature of the patient or parent or a
legal guardian covering authorization to release information are on file.
Determinations as to the release of medical and financial information
should be guided by the patient or the patient’s legal representative.
2. If patient occupied a private room or required private nursing for
medical necessity, any required certifications are on file.
3. Physician’s certifications and re-certifications, if required by contract
or Federal regulations, are on file.
4. For Religious Non-Medical facilities, verifications and if necessary re-
certifications of the patient’s need for services are on file.
5. Signature of patient or his representative on certifications,
authorization to release information, and payment request, as
required by Federal Law and Regulations (42 USC 1935f, 42 CFR
424.36, 10 USC 1071 through 1086, 32 CFR 199) and any other
applicable contract regulations, is on file.
6. The provider of care submitter acknowledges that the bill is in
conformance with the Civil Rights Act of 1964 as amended. Records
adequately describing services will be maintained and necessary
information will be furnished to such governmental agencies as
required by applicable law.
7. For Medicare Purposes: If the patient has indicated that other health
insurance or a state medical assistance agency will pay part of
his/her medical expenses and he/she wants information about
his/her claim released to them upon request, necessary authorization
is on file. The patient’s signature on the provider’s request to bill
Medicare medical and non-medical information, including
employment status, and whether the person has employer group
health insurance which is responsible to pay for the services for
which this Medicare claim is made.
8. For Medicaid purposes: The submitter understands that because
payment and satisfaction of this claim will be from Federal and State
funds, any false statements, documents, or concealment of a
material fact are subject to prosecution under applicable Federal or
State Laws.
9. For TRICARE Purposes:
(a) The information on the face of this claim is true, accurate and
complete to the best of the submitter’s knowledge and belief, and
services were medically necessary and appropriate for the health
of the patient;
(b) The patient has represented that by a reported residential address
outside a military medical treatment facility catchment area he or
she does not live within the catchment area of a U.S. military
medical treatment facility, or if the patient resides within a
catchment area of such a facility, a copy of Non-Availability
Statement (DD Form 1251) is on file, or the physician has certified
to a medical emergency in any instance where a copy of a Non-
Availability Statement is not on file;
(c) The patient or the patient’s parent or guardian has responded
directly to the provider’s request to identify all health insurance
coverage, and that all such coverage is identified on the face of
the claim except that coverage which is exclusively supplemental
payments to TRICARE-determined benefits;
(d) The amount billed to TRICARE has been billed after all such
coverage have been billed and paid excluding Medicaid, and the
amount billed to TRICARE is that remaining claimed against
TRICARE benefits;
(e) The beneficiary’s cost share has not been waived by consent or
failure to exercise generally accepted billing and collection efforts;
and,
(f) Any hospital-based physician under contract, the cost of whose
services are allocated in the charges included in this bill, is not an
employee or member of the Uniformed Services. For purposes of
this certification, an employee of the Uniformed Services is an
employee, appointed in civil service (refer to 5 USC 2105),
including part-time or intermittent employees, but excluding
contract surgeons or other personal service contracts. Similarly,
member of the Uniformed Services does not apply to reserve
members of the Uniformed Services not on active duty.
(g) Based on 42 United States Code 1395cc(a)(1)(j) all providers
participating in Medicare must also participate in TRICARE for
inpatient hospital services provided pursuant to admissions to
hospitals occurring on or after January 1, 1987; and
(h) If TRICARE benefits are to be paid in a participating status, the
submitter of this claim agrees to submit this claim to the
appropriate TRICARE claims processor. The provider of care
submitter also agrees to accept the TRICARE determined
reasonable charge as the total charge for the medical services or
supplies listed on the claim form. The provider of care will accept
the TRICARE-determined reasonable charge even if it is less
than the billed amount, and also agrees to accept the amount
paid by TRICARE combined with the cost-share amount and
deductible amount, if any, paid by or on behalf of the patient as
full payment for the listed medical services or supplies. The
provider of care submitter will not attempt to collect from the
patient (or his or her parent or guardian) amounts over the
TRICARE determined reasonable charge. TRICARE will make
any benefits payable directly to the provider of care, if the
provider of care is a participating provider.
UB-04 NOTICE: THE SUBMITTER OF THIS FORM UNDERSTANDS THAT MISREPRESENTATION OR FALSIFICATION
OF ESSENTIAL INFORMATION AS REQUESTED BY THIS FORM, MAY SERVE AS THE BASIS FOR
CIVIL MONETARTY PENALTIES AND ASSESSMENTS AND MAY UPON CONVICTION INCLUDE
FINES AND/OR IMPRISONMENT UNDER FEDERAL AND/OR STATE LAW(S).
SEE http://www.nubc.org/ FOR MORE INFORMATION ON UB-04 DATA ELEMENT AND PRINTING SPECIFICATIONS
Submission of this claim constitutes certification that the billing
information as shown on the face hereof is true, accurate and complete.
That the submitter did not knowingly or recklessly disregard or
misrepresent or conceal material facts. The following certifications or
verifications apply where pertinent to this Bill:
1. If third party benefits are indicated, the appropriate assignments by
the insured /beneficiary and signature of the patient or parent or a
legal guardian covering authorization to release information are on file.
Determinations as to the release of medical and financial information
should be guided by the patient or the patient’s legal representative.
2. If patient occupied a private room or required private nursing for
medical necessity, any required certifications are on file.
3. Physician’s certifications and re-certifications, if required by contract
or Federal regulations, are on file.
4. For Religious Non-Medical facilities, verifications and if necessary re-
certifications of the patient’s need for services are on file.
5. Signature of patient or his representative on certifications,
authorization to release information, and payment request, as
required by Federal Law and Regulations (42 USC 1935f, 42 CFR
424.36, 10 USC 1071 through 1086, 32 CFR 199) and any other
applicable contract regulations, is on file.
6. The provider of care submitter acknowledges that the bill is in
conformance with the Civil Rights Act of 1964 as amended. Records
adequately describing services will be maintained and necessary
information will be furnished to such governmental agencies as
required by applicable law.
7. For Medicare Purposes: If the patient has indicated that other health
insurance or a state medical assistance agency will pay part of
his/her medical expenses and he/she wants information about
his/her claim released to them upon request, necessary authorization
is on file. The patient’s signature on the provider’s request to bill
Medicare medical and non-medical information, including
employment status, and whether the person has employer group
health insurance which is responsible to pay for the services for
which this Medicare claim is made.
8. For Medicaid purposes: The submitter understands that because
payment and satisfaction of this claim will be from Federal and State
funds, any false statements, documents, or concealment of a
material fact are subject to prosecution under applicable Federal or
State Laws.
9. For TRICARE Purposes:
(a) The information on the face of this claim is true, accurate and
complete to the best of the submitter’s knowledge and belief, and
services were medically necessary and appropriate for the health
of the patient;
(b) The patient has represented that by a reported residential address
outside a military medical treatment facility catchment area he or
she does not live within the catchment area of a U.S. military
medical treatment facility, or if the patient resides within a
catchment area of such a facility, a copy of Non-Availability
Statement (DD Form 1251) is on file, or the physician has certified
to a medical emergency in any instance where a copy of a Non-
Availability Statement is not on file;
(c) The patient or the patient’s parent or guardian has responded
directly to the provider’s request to identify all health insurance
coverage, and that all such coverage is identified on the face of
the claim except that coverage which is exclusively supplemental
payments to TRICARE-determined benefits;
(d) The amount billed to TRICARE has been billed after all such
coverage have been billed and paid excluding Medicaid, and the
amount billed to TRICARE is that remaining claimed against
TRICARE benefits;
(e) The beneficiary’s cost share has not been waived by consent or
failure to exercise generally accepted billing and collection efforts;
and,
(f) Any hospital-based physician under contract, the cost of whose
services are allocated in the charges included in this bill, is not an
employee or member of the Uniformed Services. For purposes of
this certification, an employee of the Uniformed Services is an
employee, appointed in civil service (refer to 5 USC 2105),
including part-time or intermittent employees, but excluding
contract surgeons or other personal service contracts. Similarly,
member of the Uniformed Services does not apply to reserve
members of the Uniformed Services not on active duty.
(g) Based on 42 United States Code 1395cc(a)(1)(j) all providers
participating in Medicare must also participate in TRICARE for
inpatient hospital services provided pursuant to admissions to
hospitals occurring on or after January 1, 1987; and
(h) If TRICARE benefits are to be paid in a participating status, the
submitter of this claim agrees to submit this claim to the
appropriate TRICARE claims processor. The provider of care
submitter also agrees to accept the TRICARE determined
reasonable charge as the total charge for the medical services or
supplies listed on the claim form. The provider of care will accept
the TRICARE-determined reasonable charge even if it is less
than the billed amount, and also agrees to accept the amount
paid by TRICARE combined with the cost-share amount and
deductible amount, if any, paid by or on behalf of the patient as
full payment for the listed medical services or supplies. The
provider of care submitter will not attempt to collect from the
patient (or his or her parent or guardian) amounts over the
TRICARE determined reasonable charge. TRICARE will make
any benefits payable directly to the provider of care, if the
provider of care is a participating provider.
UB-04 NOTICE: THE SUBMITTER OF THIS FORM UNDERSTANDS THAT MISREPRESENTATION OR FALSIFICATION
OF ESSENTIAL INFORMATION AS REQUESTED BY THIS FORM, MAY SERVE AS THE BASIS FOR
CIVIL MONETARTY PENALTIES AND ASSESSMENTS AND MAY UPON CONVICTION INCLUDE
FINES AND/OR IMPRISONMENT UNDER FEDERAL AND/OR STATE LAW(S).
SEE http://www.nubc.org/ FOR MORE INFORMATION ON UB-04 DATA ELEMENT AND PRINTING SPECIFICATIONS
Submission of this claim constitutes certification that the billing
information as shown on the face hereof is true, accurate and complete.
That the submitter did not knowingly or recklessly disregard or
misrepresent or conceal material facts. The following certifications or
verifications apply where pertinent to this Bill:
1. If third party benefits are indicated, the appropriate assignments by
the insured /beneficiary and signature of the patient or parent or a
legal guardian covering authorization to release information are on file.
Determinations as to the release of medical and financial information
should be guided by the patient or the patient’s legal representative.
2. If patient occupied a private room or required private nursing for
medical necessity, any required certifications are on file.
3. Physician’s certifications and re-certifications, if required by contract
or Federal regulations, are on file.
4. For Religious Non-Medical facilities, verifications and if necessary re-
certifications of the patient’s need for services are on file.
5. Signature of patient or his representative on certifications,
authorization to release information, and payment request, as
required by Federal Law and Regulations (42 USC 1935f, 42 CFR
424.36, 10 USC 1071 through 1086, 32 CFR 199) and any other
applicable contract regulations, is on file.
6. The provider of care submitter acknowledges that the bill is in
conformance with the Civil Rights Act of 1964 as amended. Records
adequately describing services will be maintained and necessary
information will be furnished to such governmental agencies as
required by applicable law.
7. For Medicare Purposes: If the patient has indicated that other health
insurance or a state medical assistance agency will pay part of
his/her medical expenses and he/she wants information about
his/her claim released to them upon request, necessary authorization
is on file. The patient’s signature on the provider’s request to bill
Medicare medical and non-medical information, including
employment status, and whether the person has employer group
health insurance which is responsible to pay for the services for
which this Medicare claim is made.
8. For Medicaid purposes: The submitter understands that because
payment and satisfaction of this claim will be from Federal and State
funds, any false statements, documents, or concealment of a
material fact are subject to prosecution under applicable Federal or
State Laws.
9. For TRICARE Purposes:
(a) The information on the face of this claim is true, accurate and
complete to the best of the submitter’s knowledge and belief, and
services were medically necessary and appropriate for the health
of the patient;
(b) The patient has represented that by a reported residential address
outside a military medical treatment facility catchment area he or
she does not live within the catchment area of a U.S. military
medical treatment facility, or if the patient resides within a
catchment area of such a facility, a copy of Non-Availability
Statement (DD Form 1251) is on file, or the physician has certified
to a medical emergency in any instance where a copy of a Non-
Availability Statement is not on file;
(c) The patient or the patient’s parent or guardian has responded
directly to the provider’s request to identify all health insurance
coverage, and that all such coverage is identified on the face of
the claim except that coverage which is exclusively supplemental
payments to TRICARE-determined benefits;
(d) The amount billed to TRICARE has been billed after all such
coverage have been billed and paid excluding Medicaid, and the
amount billed to TRICARE is that remaining claimed against
TRICARE benefits;
(e) The beneficiary’s cost share has not been waived by consent or
failure to exercise generally accepted billing and collection efforts;
and,
(f) Any hospital-based physician under contract, the cost of whose
services are allocated in the charges included in this bill, is not an
employee or member of the Uniformed Services. For purposes of
this certification, an employee of the Uniformed Services is an
employee, appointed in civil service (refer to 5 USC 2105),
including part-time or intermittent employees, but excluding
contract surgeons or other personal service contracts. Similarly,
member of the Uniformed Services does not apply to reserve
members of the Uniformed Services not on active duty.
(g) Based on 42 United States Code 1395cc(a)(1)(j) all providers
participating in Medicare must also participate in TRICARE for
inpatient hospital services provided pursuant to admissions to
hospitals occurring on or after January 1, 1987; and
(h) If TRICARE benefits are to be paid in a participating status, the
submitter of this claim agrees to submit this claim to the
appropriate TRICARE claims processor. The provider of care
submitter also agrees to accept the TRICARE determined
reasonable charge as the total charge for the medical services or
supplies listed on the claim form. The provider of care will accept
the TRICARE-determined reasonable charge even if it is less
than the billed amount, and also agrees to accept the amount
paid by TRICARE combined with the cost-share amount and
deductible amount, if any, paid by or on behalf of the patient as
full payment for the listed medical services or supplies. The
provider of care submitter will not attempt to collect from the
patient (or his or her parent or guardian) amounts over the
TRICARE determined reasonable charge. TRICARE will make
any benefits payable directly to the provider of care, if the
provider of care is a participating provider.
UB-04 NOTICE: THE SUBMITTER OF THIS FORM UNDERSTANDS THAT MISREPRESENTATION OR FALSIFICATION
OF ESSENTIAL INFORMATION AS REQUESTED BY THIS FORM, MAY SERVE AS THE BASIS FOR
CIVIL MONETARTY PENALTIES AND ASSESSMENTS AND MAY UPON CONVICTION INCLUDE
FINES AND/OR IMPRISONMENT UNDER FEDERAL AND/OR STATE LAW(S).
SEE http://www.nubc.org/ FOR MORE INFORMATION ON UB-04 DATA ELEMENT AND PRINTING SPECIFICATIONS
Submission of this claim constitutes certification that the billing
information as shown on the face hereof is true, accurate and complete.
That the submitter did not knowingly or recklessly disregard or
misrepresent or conceal material facts. The following certifications or
verifications apply where pertinent to this Bill:
1. If third party benefits are indicated, the appropriate assignments by
the insured /beneficiary and signature of the patient or parent or a
legal guardian covering authorization to release information are on file.
Determinations as to the release of medical and financial information
should be guided by the patient or the patient’s legal representative.
2. If patient occupied a private room or required private nursing for
medical necessity, any required certifications are on file.
3. Physician’s certifications and re-certifications, if required by contract
or Federal regulations, are on file.
4. For Religious Non-Medical facilities, verifications and if necessary re-
certifications of the patient’s need for services are on file.
5. Signature of patient or his representative on certifications,
authorization to release information, and payment request, as
required by Federal Law and Regulations (42 USC 1935f, 42 CFR
424.36, 10 USC 1071 through 1086, 32 CFR 199) and any other
applicable contract regulations, is on file.
6. The provider of care submitter acknowledges that the bill is in
conformance with the Civil Rights Act of 1964 as amended. Records
adequately describing services will be maintained and necessary
information will be furnished to such governmental agencies as
required by applicable law.
7. For Medicare Purposes: If the patient has indicated that other health
insurance or a state medical assistance agency will pay part of
his/her medical expenses and he/she wants information about
his/her claim released to them upon request, necessary authorization
is on file. The patient’s signature on the provider’s request to bill
Medicare medical and non-medical information, including
employment status, and whether the person has employer group
health insurance which is responsible to pay for the services for
which this Medicare claim is made.
8. For Medicaid purposes: The submitter understands that because
payment and satisfaction of this claim will be from Federal and State
funds, any false statements, documents, or concealment of a
material fact are subject to prosecution under applicable Federal or
State Laws.
9. For TRICARE Purposes:
(a) The information on the face of this claim is true, accurate and
complete to the best of the submitter’s knowledge and belief, and
services were medically necessary and appropriate for the health
of the patient;
(b) The patient has represented that by a reported residential address
outside a military medical treatment facility catchment area he or
she does not live within the catchment area of a U.S. military
medical treatment facility, or if the patient resides within a
catchment area of such a facility, a copy of Non-Availability
Statement (DD Form 1251) is on file, or the physician has certified
to a medical emergency in any instance where a copy of a Non-
Availability Statement is not on file;
(c) The patient or the patient’s parent or guardian has responded
directly to the provider’s request to identify all health insurance
coverage, and that all such coverage is identified on the face of
the claim except that coverage which is exclusively supplemental
payments to TRICARE-determined benefits;
(d) The amount billed to TRICARE has been billed after all such
coverage have been billed and paid excluding Medicaid, and the
amount billed to TRICARE is that remaining claimed against
TRICARE benefits;
(e) The beneficiary’s cost share has not been waived by consent or
failure to exercise generally accepted billing and collection efforts;
and,
(f) Any hospital-based physician under contract, the cost of whose
services are allocated in the charges included in this bill, is not an
employee or member of the Uniformed Services. For purposes of
this certification, an employee of the Uniformed Services is an
employee, appointed in civil service (refer to 5 USC 2105),
including part-time or intermittent employees, but excluding
contract surgeons or other personal service contracts. Similarly,
member of the Uniformed Services does not apply to reserve
members of the Uniformed Services not on active duty.
(g) Based on 42 United States Code 1395cc(a)(1)(j) all providers
participating in Medicare must also participate in TRICARE for
inpatient hospital services provided pursuant to admissions to
hospitals occurring on or after January 1, 1987; and
(h) If TRICARE benefits are to be paid in a participating status, the
submitter of this claim agrees to submit this claim to the
appropriate TRICARE claims processor. The provider of care
submitter also agrees to accept the TRICARE determined
reasonable charge as the total charge for the medical services or
supplies listed on the claim form. The provider of care will accept
the TRICARE-determined reasonable charge even if it is less
than the billed amount, and also agrees to accept the amount
paid by TRICARE combined with the cost-share amount and
deductible amount, if any, paid by or on behalf of the patient as
full payment for the listed medical services or supplies. The
provider of care submitter will not attempt to collect from the
patient (or his or her parent or guardian) amounts over the
TRICARE determined reasonable charge. TRICARE will make
any benefits payable directly to the provider of care, if the
provider of care is a participating provider.
UB-04 NOTICE: THE SUBMITTER OF THIS FORM UNDERSTANDS THAT MISREPRESENTATION OR FALSIFICATION
OF ESSENTIAL INFORMATION AS REQUESTED BY THIS FORM, MAY SERVE AS THE BASIS FOR
CIVIL MONETARTY PENALTIES AND ASSESSMENTS AND MAY UPON CONVICTION INCLUDE
FINES AND/OR IMPRISONMENT UNDER FEDERAL AND/OR STATE LAW(S).
SEE http://www.nubc.org/ FOR MORE INFORMATION ON UB-04 DATA ELEMENT AND PRINTING SPECIFICATIONS



