Fillable Printable Medical Group Medical History Form - Oregon
Fillable Printable Medical Group Medical History Form - Oregon
Medical Group Medical History Form - Oregon
Oregon Medical Group
Medical History Form
4032-00 12/09 Page 1 of 4
What areas or issues would you like to discuss today: (Please limit to 3 items)
1. ___________________________________________ 2. ______________________________________________________
3. _____________________________________________________________________________________________________
PREVENTATIVE HEALTH STATUS:
Date of last physical exam: ________________ Last eye exam: ________________ Last dental exam: ________________
Have you ever had a colonoscopy or sigmoidoscopy? yes no When/Findings: _____________________________
Have you ever had a bone density test? yes no When/Findings: _______________________________________
Do you have an Advance Directive for health care decisions? yes no
Last immunizations: (please give date of most recent vaccination or series completion date)
Tetanus: ___________ Hepatitis B: ___________ Hepatitis A: ___________ HPV: ___________ Influenza: ___________
Pneumonia: ___________ Shingles: ___________ TB skin test result: _________________________ Date: ___________
FOR WOMEN ONLY:
Date of last period: ___________ Last Pap: ___________ Age periods began: ______ Age at start of menopause: ______
Have you had a mammogram? yes no Most recent date ___________ Result _____________________________
Birth control method: ________________________________________________________________________________
Have you had any pregnancies? yes no Total number ____________Miscarriages/Abortions ________________
Problems during pregnancies: __________________________________________________________________________
FOR MEN ONLY:
Have you had a PSA blood test and/or prostate exam? yes no Last Date __________ Result__________________
SOCIAL HISTORY:
Occupation: _______________________________ Former Regions of Residence: _______________________________
Marital Status: Single Married Domestic Partnership Divorced Widowed
Living Situation: Alone Roommate Spouse Parents Significant Other With Children
Have you been in a relationship where you were hurt, threatened or made to feel afraid? yes no
Do you drink alcohol? yes no How many per week? __________________ Quit/When ________________
Do you use tobacco? yes no How much/how long? __________________ Quit/When ________________
Do you drink caffeine? yes no How much per day? _____________________________________________
Have you used drugs? yes no Which ones? _________________________ Quit/When ________________
Do you exercise? yes no Type: _______________________ How often? _____________________
Do you follow a diet? yes no Please describe: ________________________________________________
Date _____________ Patient Name _______________________________ Age ______ Date of Birth ______________
Other Physicians involved in my care ___________________________________________________________________
Referred to this office by _____________________________________________________________________________

Oregon Medical Group
Medical History Form
4032-00 12/09 Page 2 of 4
Today’s Date _____________ Patient Name ________________________________ Date of Birth ______________
PERSONAL MEDICAL HISTORY: Have you ever been diagnosed with the following? (Please circle)
Heart Disease:
murmur
angina / coronary disease
congestive heart failure
rheumatic fever
valve replacement
irregular heartbeat
heart attack
high blood pressure
Infectious Disease:
AIDS or HIV positive
MRSA infection
tuberculosis
sexually transmitted disease
Musculoskeletal:
rheumatoid arthritis
gout
osteoarthritis
fibromyalgia
Gynecological:
abnormal pap
endometriosis
fibroids
ovarian cysts
irregular bleeding
Respiratory:
asthma
allergies / hay fever
emphysema/COPD
chronic bronchitis
pneumonia
asbestos exposure
sleep apnea
Gastrointestinal:
ulcers
colon polyps
gallstones
hiatal hernia
hepatitis, type _________
hemorrhoids
irritable bowel syndrome
colitis
diverticulosis
gastrointestinal bleeding
Kidney/Bladder:
stones
prostate disorder
incontinence
infection
Mental Health/Neurologic:
anxiety
depression
alcoholism
drug abuse
other mental illness
migraines/headaches
stroke
seizures
paralysis
Metabolic/Nutrition:
diabetes
high cholesterol
anemia
thyroid problem
bleeding disorder
Cancer:
breast cancer
cervical cancer
ovarian cancer
colon cancer
skin cancer
prostate cancer
other cancer (type) ________
______________________
None of the above
Have you ever had a blood transfusion? yes no If yes, when? ______________________________________
Childhood Illnesses: ___________________________________________________________________________________
Hospitalizations, operations, serious illnesses or injuries: (omit pregnancies)
Date Date
1. ____________________________________________________ 3. __________________________________________________
2. ____________________________________________________ 4. __________________________________________________
Present Medications: (Include birth control pills and non-prescriptive items such as vitamins, aspirin, herbs, etc.)
Name Dose Times/Day Name Dose Times/Day
1. _____________________________ ________ __________ 5. _____________________________ ________ __________
2. _____________________________ ________ __________ 6. _____________________________ ________ __________
3. _____________________________ ________ __________ 7. _____________________________ ________ __________
4. _____________________________ ________ __________ 8. _____________________________ ________ __________
Drug Allergies:
Medication Type of Reaction Medication Type of Reaction
1. _____________________________ _____________________ 3. _____________________________ _____________________
2. _____________________________ _____________________ 4. _____________________________ _____________________
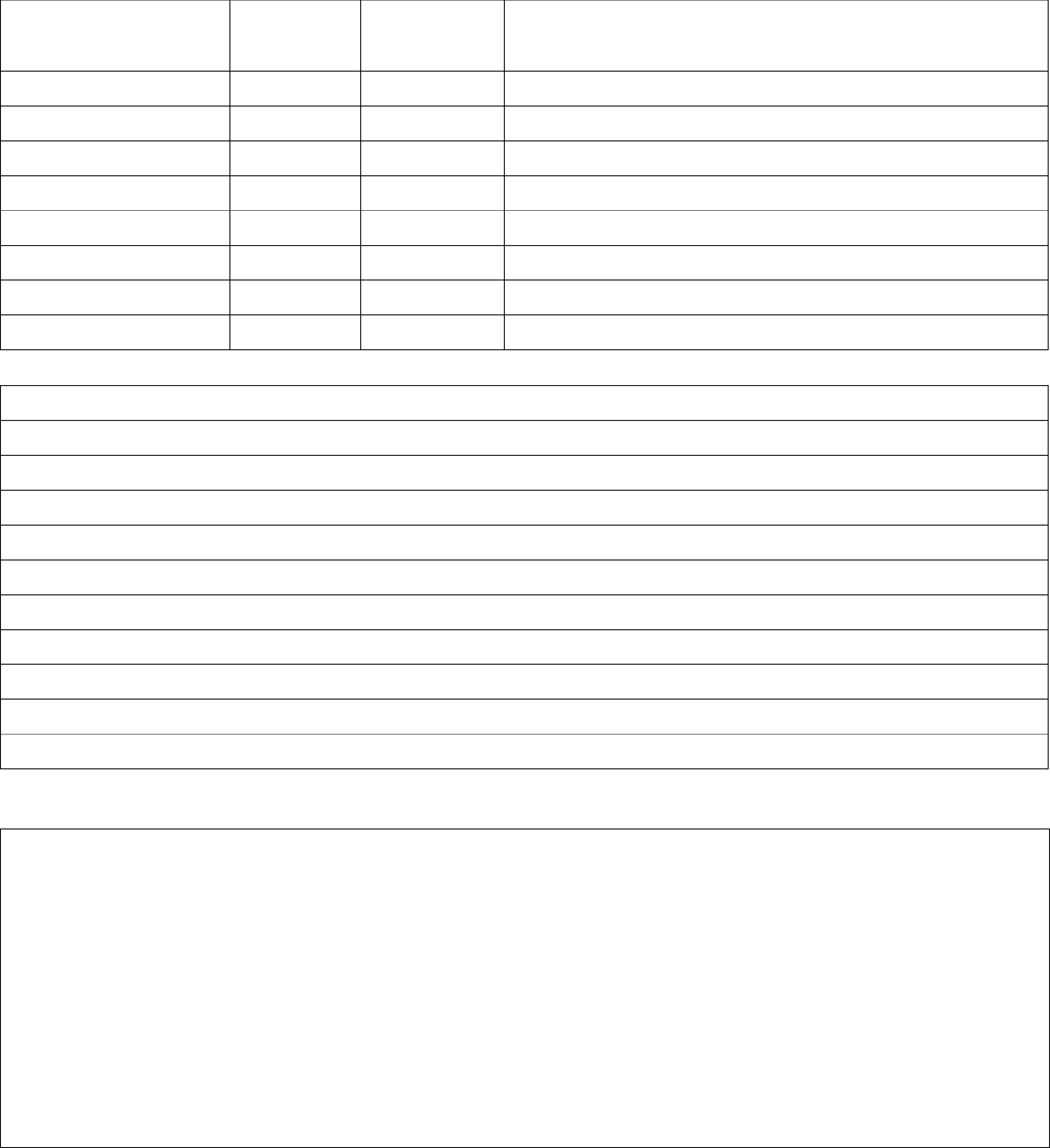
Oregon Medical Group
Medical History Form
4032-00 12/09 Page 3 of 4
Today’s Date _____________ Patient Name ________________________________ Date of Birth ______________
FAMILY HISTORY
Relation
If Living:
Age
If Deceased:
Age at Death
Cause
Father
Mother
Brother or sister
1.
2.
3.
4.
5.
Has any of your immediate family ever had: (if yes, indicate relationship and age of onset)
Allergy/Asthma
Arthritis/Gout
Cancer
Depression
Diabetes
Epilepsy/Seizures
Glaucoma
Heart Disease/Coronary Artery Disease
High Blood Pressure
Liver Disease
Kidney Disease
Mental Illness
Alcohol/Substance Abuse
Migraine Headaches
Overweight
High Cholesterol
Stroke
Thyroid Disease
Tuberculosis
Ulcers
Bleeding Disorder
Colon Polyps
Other family medical history: ___________________________________________________________________________
For Clinician Use
Oregon Medical Group
Medical History Form
4032-00 12/09 Page 4 of 4
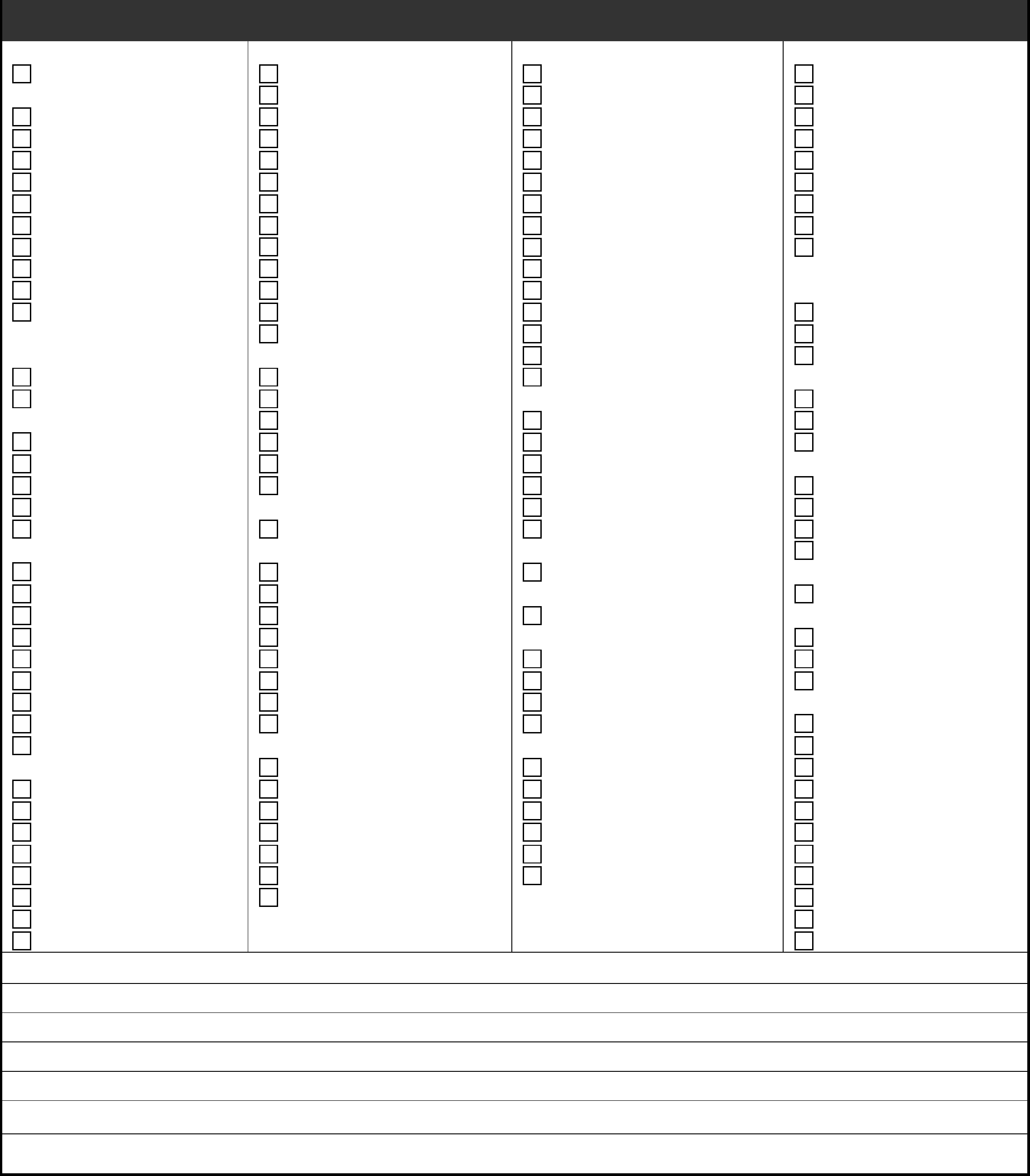
Today’s Date _____________ Patient Name __________________________________ Date of Birth ________________
REVIEW OF SYSTEMS: Check any of the following symptoms you have experienced WITHIN THE PAST YEAR
GENERAL:
change in heat & cold
tolerance
persistent fever
chills/cold intolerance
excess appetite
increased thirst
lack of appetite
night sweats
swollen glands
unusual weakness
unusual fatigue
weight change
increase ___
decrease ___
Other _______________
None of the above
ALLERGY:
sneezing
environmental allergy
food allergy ___________
Other ________________
None of the above
SKIN:
ulcers
bruise easily
change in skin or mole
dryness of skin
rash or hives
nail change
unusual hair loss
Other _______________
None of the above
EYES:
eye pain
blind spells (in one eye)
change in vision
contact lenses
eye infection
wear glasses
Other _______________
None of the above
EARS/NOSE/THROAT:
earache
hearing loss
ear infection or drainage
ringing in ears
bleeding gums
hoarseness
neck swelling/lumps
sores in mouth
nose bleeds
nasal polyps
sinus trouble
Other _________________
None of the above
BREASTS:
discharge/bleeding
nipple changes
lump
pain
Other _________________
None of the above
HEART:
white, blue or purple
discoloration of hands or feet
calf pain when walking
chest discomfort/pain
irregular heart beat
racing or fluttering heart
swollen feet or ankles
varicose veins
Other _________________
None of the above
LUNGS:
shortness of breath
persistent cough
wheezing
cough up blood
cough up phlegm
difficulty breathing
None of the above
GASTROINTESTINAL:
belching
bloody or black stools
change in stools
constipation
difficult swallowing
excessive gas
food intolerance
heartburn/esophageal reflux
hemorrhoids
loose bowels/diarrhea
nausea
recurrent abdominal pain
vomiting
Other ________________
None of the above
URINARY:
change in urinary stream
blood in urine
difficulty urinating
frequency
leaking urine
pain or burning on
urination
unusually large volumes
of urine
up at night to urinate?
how often? ___________
incontinence
sexual difficulty
Other _______________
None of the above
FEMALE:
heavy menstrual bleeding
irregular menstrual periods
discharge
premenstrual symptoms
Other ________________
None of the above
BONES AND JOINTS:
back or neck pain
cramps in muscles
painful or stiff joints
pain down backs of legs
pain in legs with walking
swelling in legs
redness of joints
Other ______________
None of the above
MOOD/MENTAL
HEALTH:
depressed or sad
irritable or angry
anxious, tense, or
worried
fearful
sleep problems
loss of interest in
activities
fatigue
suicidal thoughts
compulsive behaviors
concentration/memory
problems
marital, family or
work problems
stress
Other ______________
None of the above
NEUROLOGIC:
coordination problems
difficulties in speaking
dizziness
fainting spells
frequent headaches
loss of balance
loss of sensation
muscle weakness
numbness or tingling
Other ______________
None of the above
For Clinician Use
Reviewed by
Date



