- Direct Reimbursement Calim Form - University of Virginia
- Member Reimbursement Form for Medical Claims and Prescription Drugs
- Medical Care Reimbursement Request - Dartmouth College
- Medical Reimbursement Form - Florida
- CLAIM FOR REIMBURSEMENT OF MEDICAL EXPENSES
- Member Reimbursement Medical Claim Form
Fillable Printable Member Reimbursement Form for Medical Claims and Prescription Drugs
Fillable Printable Member Reimbursement Form for Medical Claims and Prescription Drugs
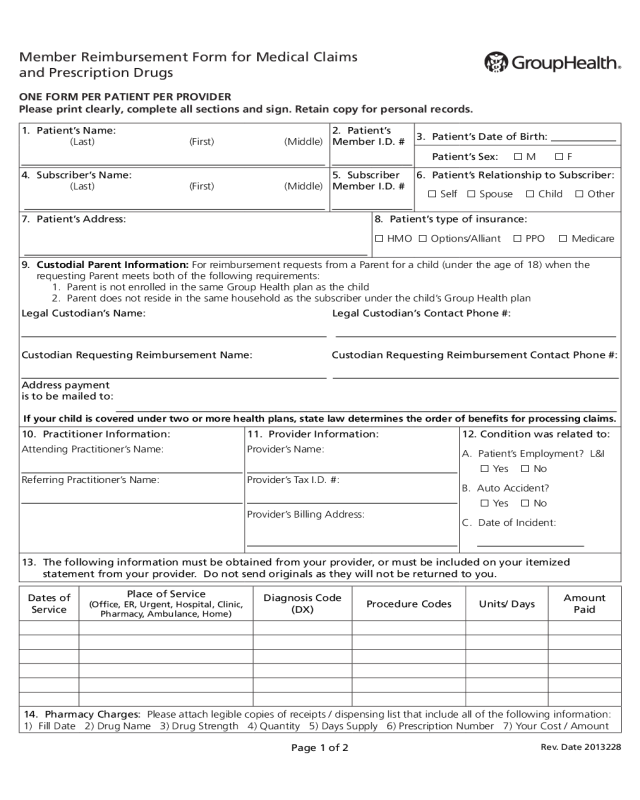
Member Reimbursement Form for Medical Claims and Prescription Drugs
Member Reimbursement Form for Medical Claims
and Prescription Drugs
ONE FORM PER PATIENT PER PROVIDER
Please print clearly, complete all sections and sign. Retain copy for personal records.
1. Patient’s Name:
(Last) (First) (Middle)
2. Patient’s
Member I.D. #
3. Patient’s Date of Birth:
Patient’s Sex: M F
4. Subscriber’s Name:
(Last) (First) (Middle)
5. Subscriber
Member I.D. #
6. Patient’s Relationship to Subscriber:
Self Spouse Child Other
7. Patient’s Address:
8. Patient’s type of insurance:
HMO Options/Alliant PPO Medicare
9. Custodial Parent Information: For reimbursement requests from a Parent for a child (under the age of 18) when the
requesting Parent meets both of the following requirements:
1. Parent is not enrolled in the same Group Health plan as the child
2. Parent does not reside in the same household as the subscriber under the child’s Group Health plan
Legal Custodian’s Name: Legal Custodian’s Contact Phone #:
Custodian Requesting Reimbursement Name: Custodian Requesting Reimbursement Contact Phone #:
Address payment
is to be mailed to:
If your child is covered under two or more health plans, state law determines the order of benefits for processing claims.
10. Practitioner Information:
Attending Practitioner’s Name:
Referring Practitioner’s Name:
11. Provider Information:
Provider’s Name:
Provider’s Tax I.D. #:
Provider’s Billing Address:
12. Condition was related to:
A. Patient’s Employment? L&I
Yes No
B. Auto Accident?
Yes No
C. Date of Incident:
13. The following information must be obtained from your provider, or must be included on your itemized
statement from your provider. Do not send originals as they will not be returned to you.
Dates of
Service
Place of Service
(Office, ER, Urgent, Hospital, Clinic,
Pharmacy, Ambulance, Home)
Diagnosis Code
(DX)
Procedure Codes Units/ Days
Amount
Paid
14. Pharmacy Charges: Please attach legible copies of receipts / dispensing list that include all of the following information:
1) Fill Date 2) Drug Name 3) Drug Strength 4) Quantity 5) Days Supply 6) Prescription Number 7) Your Cost / Amount
Rev. Date 2013228
Page 1 of 2
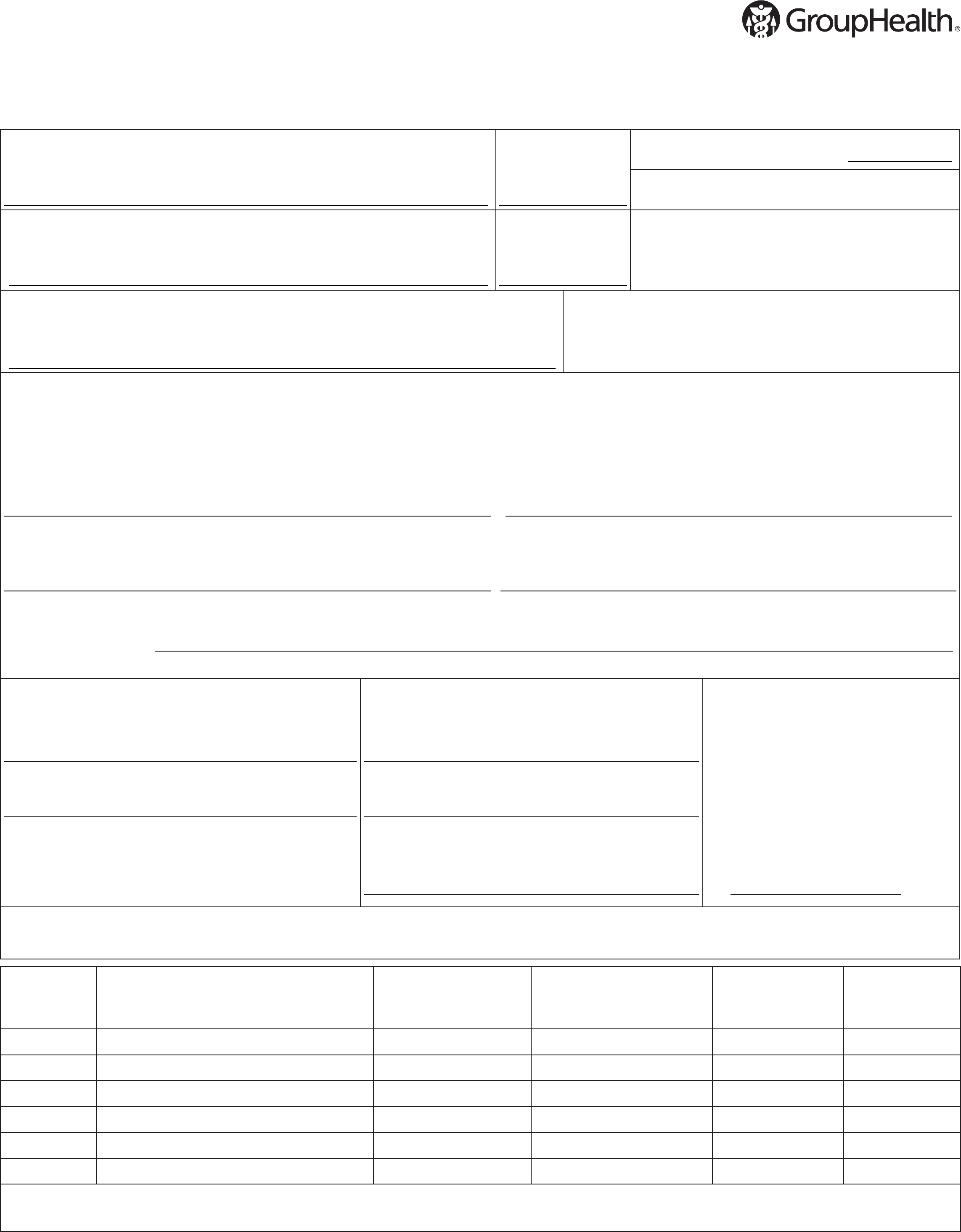
15. Foreign Claims:
For services out of country, please provide name of country:
Where services were rendered: Office/ Clinic ER Urgent Care Hospital Pharmacy
Please explain injury or illness:
Itemized bills, receipts, and statements must be translated prior to submittal. Translation will be at the members expense.
16. I have attached one of the
following proof of payments:
The front and back of the cleared
check written to the provider, or
bank encoded copy of the front
check written to the provider.
A copy of a credit card statement
that includes the charges and the
provider’s name.
A copy of the receipt, with the
provider’s name and address
preprinted on the receipt.
Note: Itemized statements/ invoices
do not count as proof of payment.
17. Information about payment(s)
made:
Was there a discount for the services?
Yes No
If Yes, is the amount paid after the discount?
Yes No
Is there a balance due?
Yes No
Note: if there is a balance due to the provider
you may not be entitled to a refund.
18. Other Insurance information:
Is the patient covered by another health
plan? Yes No
Subscriber name for other insurance:
Name of other insurance company:
Did other insurance make a payment?
Yes No
If yes, include Explanation of Benefits
from other insurance plan(s).
19. Signature is required:
I attest that the above information is true and accurate, and the services were received and paid for in the amount requested as
indicated above. I acknowledge that if any information on this form is misleading or fraudulent, my coverage may be cancelled and
I may be subject to criminal and / or civil penalties for false health care claims.
Signature: Date:
For any questions please contact Customer Service toll-free at 1-888-901-4636, (TTY Relay: 711 or 1-800-833-6388). Or visit ghc.
org, click on “Customer Service” and send an email.
Reimbursement requests will be processed within 45 days of receipt.
Itemized receipts, invoices, and proof of payment must be submitted, otherwise form may be sent back for lack of information.
Submit all documents to:
Claims Processing
Group Health Cooperative
PO Box 34585
Seattle, WA 98124-1585
Member Reimbursement Form for Medical Claims and Prescription Drugs Instructions
Please complete all items on the claim form. If the information requested does not apply to the patient, indicate N/A (Not Applicable). Special
care should be taken when completing the following sections:
10. Practitioner Information – Please fill out attending practitioner’s name with the physician that was seen for services. Please fill referring
practitioner’s name with the physician that referred you if applicable.
11.
Provider Information – Please fill out provider name with the name of the facility that was visited. Please fill out Provider Tax ID with the
facility’s Tax ID (this number will need to be obtained from the provider). Please fill out provider billing address with the facility’s address.
12. Condition was related to – Please indicate if the injury or reason of visit was related to your employment (L&I), or an auto accident, and
if yes to either of them please indicate the date of accident.
13. Itemization – This information must be obtained from your provider, or must be included on your itemized statement from your
provider. If this information is included on your itemized statement you can state please review attached itemized statement.
14. Pharmacy Charges – Please attach legible copies of receipts / dispensing lists that include fill date, drug name, drug strength, quantity,
days supply, prescription number, and your cost / amount paid.
15. Foreign Claims – Please complete this section if your services were completed outside of the country, otherwise indicate N/A.
16. Proof of payment – Please indicate what type of proof of payment you have attached with this form.
17. Payment information – Please answer each question by checking the box that applies to the payment(s) you made to the provider.
18. Other insurance – Please indicate whether you have coverage from another insurance, if applicable the name of the subscriber for the
other insurance and the name of the other insurance, and indicate by checking the box if they made a payment.
19. Signature – This form must be signed and dated by either the subscriber or the patient.
Page 2 of 2



