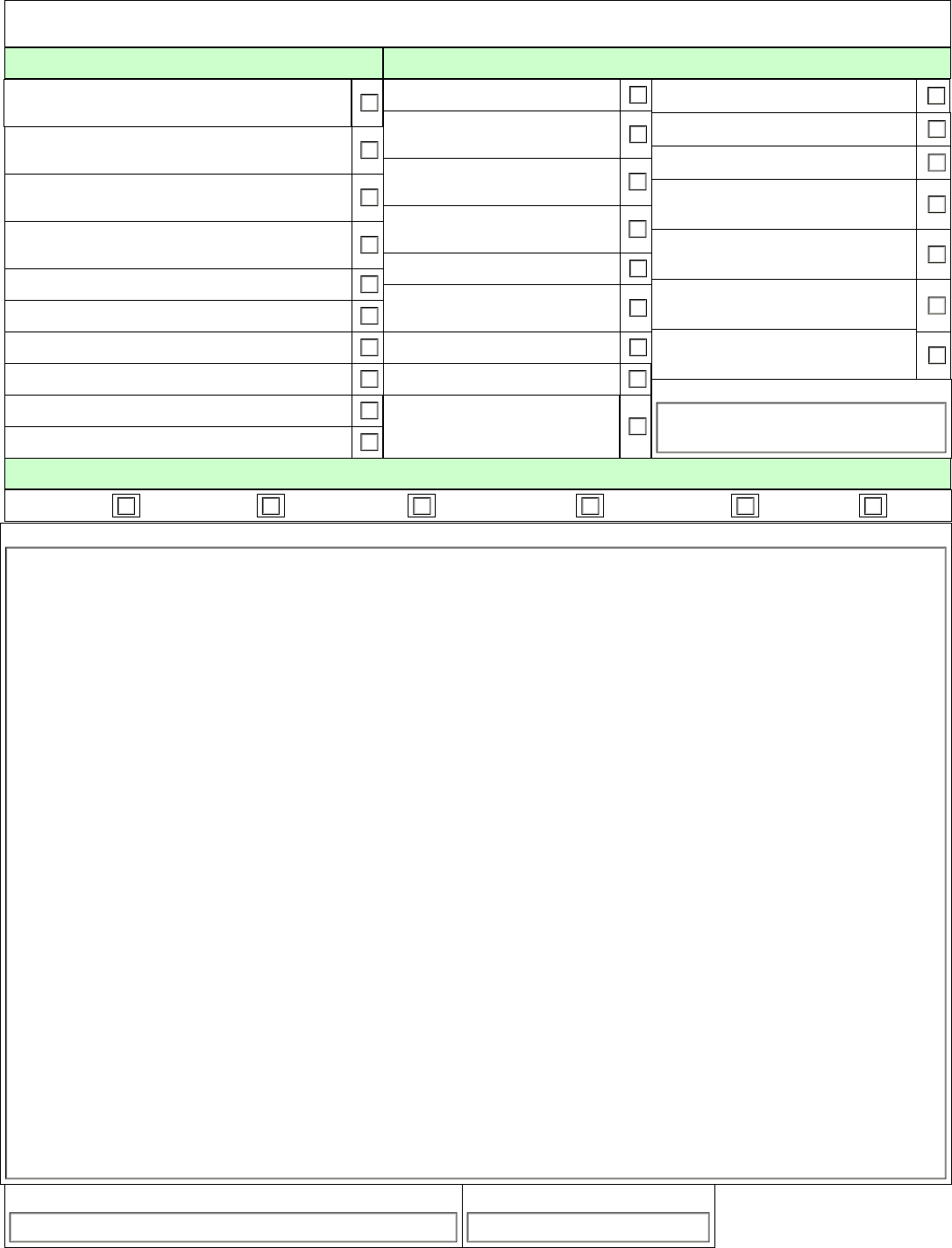
Fillable Printable VA Form 10-0415
Fillable Printable VA Form 10-0415
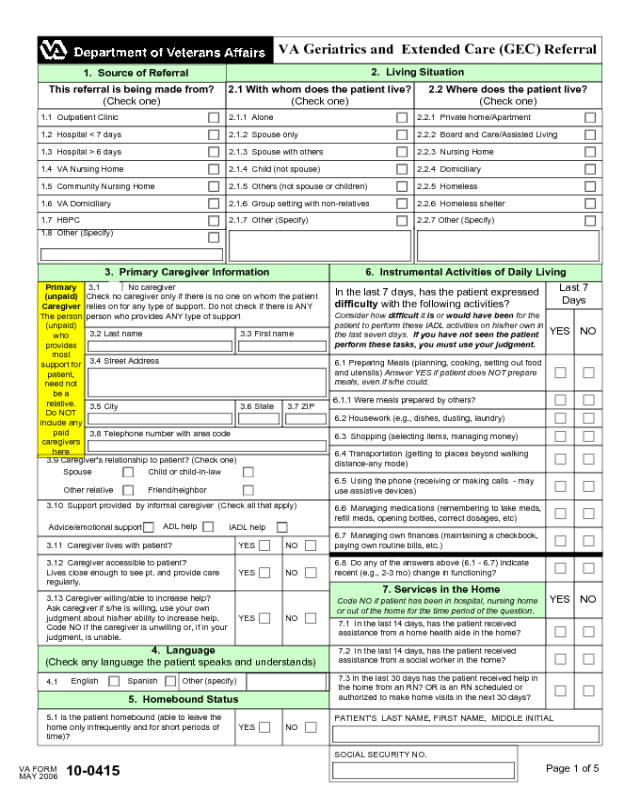
VA Form 10-0415
VA Geriatrics and Extended Care (GEC) Referral
3.2 Last name
1. Source of Referral
2. Living Situation
This referral is being made from?
(Check one)
2.1 With whom does the patient live?
(Check one)
2.2 Where does the patient live?
(Check one)
1.1 Outpatient Clinic 2.1.1 Alone 2.2.1 Private home/Apartment
1.2 Hospital < 7 days
1.3 Hospital > 6 days
1.4 VA Nursing Home
1.5 Community Nursing Home
1.6 VA Domiciliary
1.7 HBPC
1.8 Other (Specify)
2.1.2 Spouse only
2.1.3 Spouse with others
2.1.4 Child (not spouse)
2.1.5 Others (not spouse or children)
2.1.6 Group setting with non-relatives
2.1.7 Other (Specify)
2.2.2 Board and Care/Assisted Living
2.2.3 Nursing Home
2.2.4 Domiciliary
2.2.5 Homeless
2.2.6 Homeless shelter
2.2.7 Other (Specify)
3. Primary Caregiver Information 6. Instrumental Activities of Daily Living
Primary
(unpaid)
Caregiver
The person
(unpaid)
who
provides
most
support for
patient,
need not
be a
relative.
Do NOT
include any
paid
caregivers
here
3.1 No caregiver
Check no caregiver only if there is no one on whom the patient
relies on for any type of support. Do not check if there is ANY
person who provides ANY type of support
3.3 First name
3.4 Street Address
3.5 City 3.6 State 3.7 ZIP
3.8 Telephone number with area code
In the last 7 days, has the patient expressed
difficulty with the following activities?
Consider how difficult it is or would have been for the
patient to perform these IADL activities on his/her own in
the last seven days. If you have not seen the patient
perform these tasks, you must use your judgment.
Last 7
Days
YES NO
6.1 Preparing Meals (planning, cooking, setting out food
and utensils) Answer YES if patient does NOT prepare
meals, even if s/he could.
6.1.1 Were meals prepared by others?
6.2 Housework (e.g., dishes, dusting, laundry)
6.3 Shopping (selecting items, managing money)
6.4 Transportation (getting to places beyond walking
distance-any mode)
6.5 Using the phone (receiving or making calls - may
use assistive devices)
3.9 Caregiver's relationship to patient? (Check one)
Spouse Child or child-in-law
Friend/neighbor
Other relative
6.6 Managing medications (remembering to take meds,
refill meds, opening bottles, correct dosages, etc)
6.7 Managing own finances (maintaining a checkbook,
paying own routine bills, etc.)
6.8 Do any of the answers above (6.1 - 6.7) indicate
recent (e.g., 2-3 mo) change in functioning?
3.10 Support provided by informal caregiver (Check all that apply)
3.11 Caregiver lives with patient?
Advice/emotional support
ADL help
IADL help
7. Services in the Home
Code NO if patient has been in hospital, nursing home
or out of the home for the time period of the question.
3.12 Caregiver accessible to patient?
Lives close enough to see pt. and provide care
regularly.
3.13 Caregiver willing/able to increase help?
Ask caregiver if s/he is willing, use your own
judgment about his/her ability to increase help.
Code NO if the caregiver is unwilling or, if in your
judgment, is unable.
7.1 In the last 14 days, has the patient received
assistance from a home health aide in the home?
7.2 In the last 14 days, has the patient received
assistance from a social worker in the home?
7.3 In the last 30 days has the patient received help in
the home from an RN? OR is an RN scheduled or
authorized to make home visits in the next 30 days?
4. Language
(Check any language the patient speaks and understands)
4.1
English Spanish
Other (specify)
5. Homebound Status
5.1 Is the patient homebound (able to leave the
home only infrequently and for short periods of
time)?
NOYES
PATIENT'S LAST NAME, FIRST NAME, MIDDLE INITIAL
SOCIAL SECURITY NO.
NOYES
NOYES
NO
YES
NOYES
MAY 2006
VA FORM
10-0415
Page 1 of 5
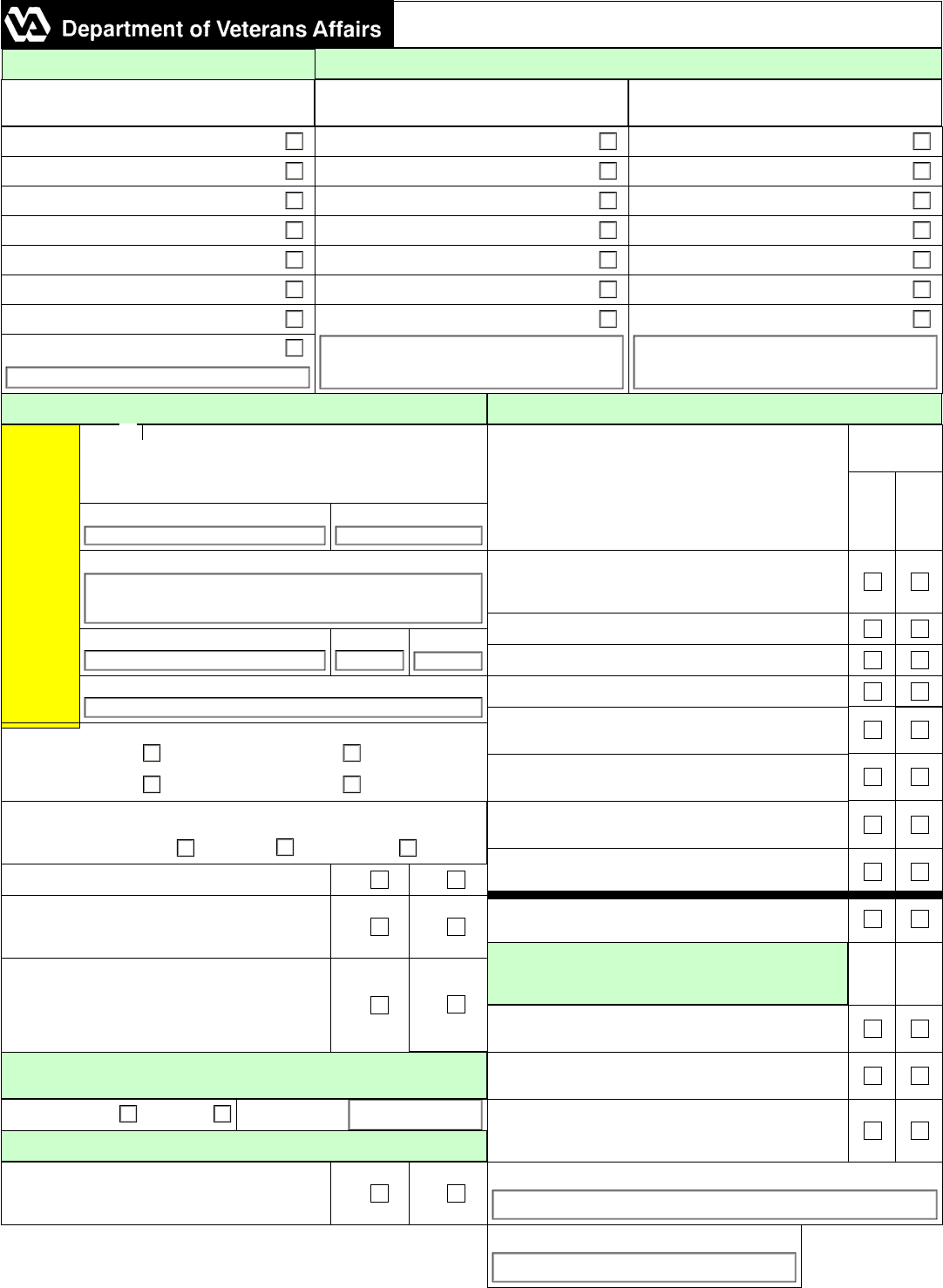
8.7 Has the patient completed an Advance Directive? (If yes, please place copy in Medical Record or send with patient)
9.16 Check the stage of the worst pressure ulcer
1 2 3 4
8.6 Does the veteran have a substitute (surrogate) decision-maker designated? (Check any that apply, include names when available)
8. Additional Information
VA Geriatrics and Extended Care (GEC) Referral con't
NOYES
NOYES
8.1 In the last 90 days, has the patient moved in with others or have others moved in with the patient?
8.2 Are there any hazards or other factors that make it difficult for the patient to enter or leave the home? Any environmental factor e.
g., environmental factors such as stairs, broken elevators, etc., that make it difficult to leave the home (do not count poor
lighting or loose rugs/carpet)
8.3 Does the patient or primary caregiver believe the patient would be better off in another living environment?
8.4 In the last 7 days, did the patient engage in 2 or more hours of physical activity, e.g.,
walking, cleaning the house or exercising?
YES, Performed for 2 or more hours
NO, not performed or less than 2 hours
8.5 In the last 7 days, has the patient been left alone in the mornings or afternoons?
YES, Occasionally alone, even if only for an hour
NO, Never or hardly ever
Guardian
Fiduciary/Conservator
Durable Power of Attorney
Health Care
Financial
9. Skilled Care
10. Basic Activities of Daily Living
Code YES if the patient had ANY difficulty, required cueing or
supervision, or DID NOT do the task in the last 7 days
Will the patient require these treatments after
referral?
YES
9.1 CPAP/BiPap or Ventilator
9.2 Oxygen
9.3 Suctioning
9.9 IV Infusions
9.4 Tracheostomy Care
9.5 Ostomy Care (other than tracheostomy)
9.6 Dysphagia Diet
9.7 Tube Feeding (any method)
9.8 Parenteral Feeding
9.10 Medications by Injection
9.11 Urinary Catheter Care
9.12 Dialysis - Center- based
9.13 Dialysis - Home -based
9.14 Wound Care (other than pressure ulcer)
9.15 Pressure Ulcer Care
9.17 Frequent Nurse Observation (more than 1/
week)
9.18 Physical, Speech, Occupational or
Kinesiotherapy
9.19 Alcohol, Drug, or other substance abuse
treatment
9.20 Other
(specify)
In the last 7 days, has the patient required help OR supervision to
perform any of the following activities?
Last 7
Days
NOYES
10.1 Bathing (tub bath, shower, or sponge)
10.1.1 Did the patient require physical assistance with bathing?
10.2 Dressing (lower and upper body)
10.3 Eating (taking in food by any method, including tube feedings)
10.4 Using the toilet (using toilet, urinal, bedpan-getting on and off,
cleaning self, managing devices used and adjusting clothes)
10.5 Moving around in bed (moving to and from lying position, turning
side to side, repositioning)
10.6 Transfers (moving to/from bed, chair, wheelchair, standing)
10.7 Moving around indoors (Answer yes even if with cane, walker, or
scooter - Answer NO if uses wheelchair OR did not get around
10.8 If uses wheelchair, moving around chair (propelling and
maneuvering) Code YES if the patient can maneuver wheelchair by
him/herself (even if it is a power chair)
11.1 Is the patient incontinent of urine?
10.9 Do any of the answers above (10-1 - 10-7) indicate a recent (2-3
mos) change in functioning? Code yes if the patient's function has
significantly changed in the recent past
11. CONTINENCE NOYES
11.2 Is the patient incontinent of stool?
12. SKIN NOYES
12.1 Has the patient experienced any troubling skin problems like
burns, bruises, or itching in the last 30 days?
Additional comments pertinent
to this page have been added
PATIENT'S LAST NAME, FIRST NAME, MIDDLE INITIAL SOCIAL SECURITY NO.
YES NO
MAY 2006
VA FORM
10-0415
Page 2 of 5
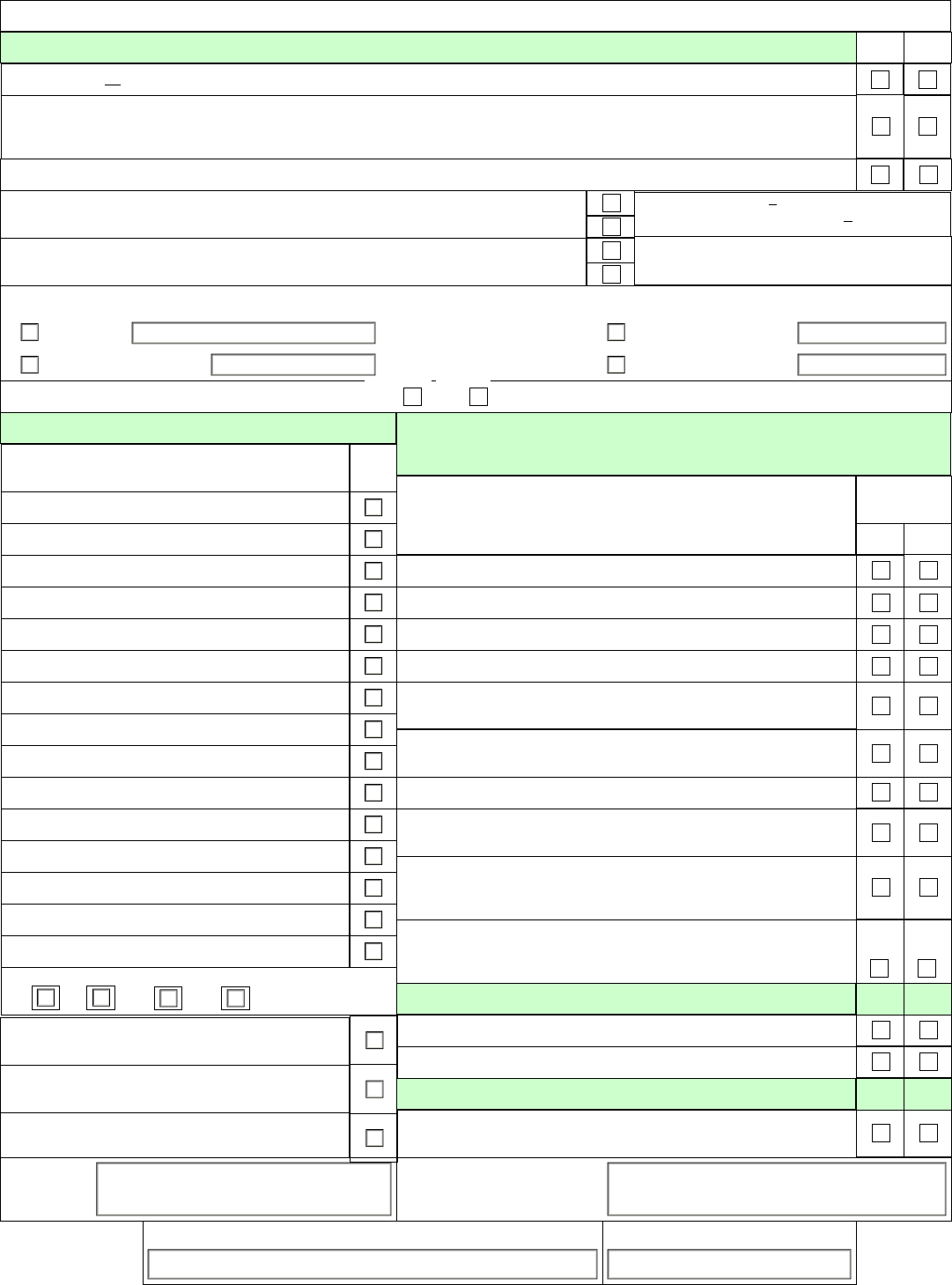
I7.1 Diet Regular Modified (Specify diet)
In the last 7 days, has the patient exhibited any of the following?
13. Patient Behaviors and Symptoms
VA Geriatrics and Extended Care (GEC) Referral con't
Last 7
Days
NOYES
I3.1 Wandering (moved with no rational purpose, seemingly oblivious to needs or safety)? Wandering is purposeless movement often
without regard to safety. Pacing up and down is NOT wandering.
I3.2 Verbally abusive behaviors (threatened, screamed at, or cursed at others)? Code if any such behavior occurred, regardless of
patient's intent.
I3.3 Physically abusive behaviors (hit, shoved, scratched or sexually abused others)? Code if any such behavior occurred, regardless
of patient's intent.
I3.4 Resisting care (resisted taking medications /injections, ADL assistance, eating, or changes in position)?
I3.5 Hallucinations or delusions? Hallucinations are sensory (auditory, visual, olfactory, tactile) experiences that are NOT real
Delusions are ideas or beliefs that are held even though there is no evidence to support them or evidence that shows them to be
false.
14.1 In the last 7 days was the patient able, without difficulty, to
make decisions that are reasonable about organizing the day,
such as when to get up, what meals to have or what clothes to
wear?
14. Cognitive Status
I4.2 In the last 7 days, has the patient usually been able to make
him/herself understood?
I4.3 In the last 90 days has the person become so agitated or disoriented that his safety was endangered or s/he required protection
by others as a result?
YES, Patient consistently made reasonable decisions without difficulty
NO, Patient made decisions with difficulty OR did not make decisions
OR decisions were poor
YES, Patient's expression of information is understood, even if s/he has
difficulty in finding words or finishing thoughts
NO, Patient's expression of information is never (or rarely) understood
OR s/he is limited to making concrete requests
15. Prognosis
I5.1 In the last 7 days, has the person experienced a flare up of a recurrent or chronic health problem?
I5.2 Does the direct care staff (MD, rehab therapist) think the patient is capable of increased independence (in ADLs, IADLs, or
mobility)?
I5.3 Does the patient have a limited life expectancy (likely to be less than 6 months)?
16. Weight Bearing
I6.1 What is the patient's weight bearing status? Full Partial None
17. Diet
18. What equipment does the patient need? (Please place prosthetics requests)
18.1 Hospital Bed
18.2 Special mattress
18.3 Trapeze 18.5 Cane 18.7 ADL equipment
18.4 Walker 18.8 Orthotic or splint18.6 Wheelchair
18.9 Other (specify)
19. What supplies does the patient need? (Please place orders for supplies)
19.1 Catheters
19.2 Tubing
19.3 Dressings 19.5 Tape 19.7 Ostomy supplies
19.4 Wrappings 19.8 Saline 19.6 Glucose strips
19.9 Other (specify)
SOCIAL SECURITY NO.PATIENT'S LAST NAME, FIRST NAME, MIDDLE INITIAL
YES
NO
NO
YES
NO
YES
NO
YES
MAY 2006
VA FORM
10-0415
Page 3 of 5
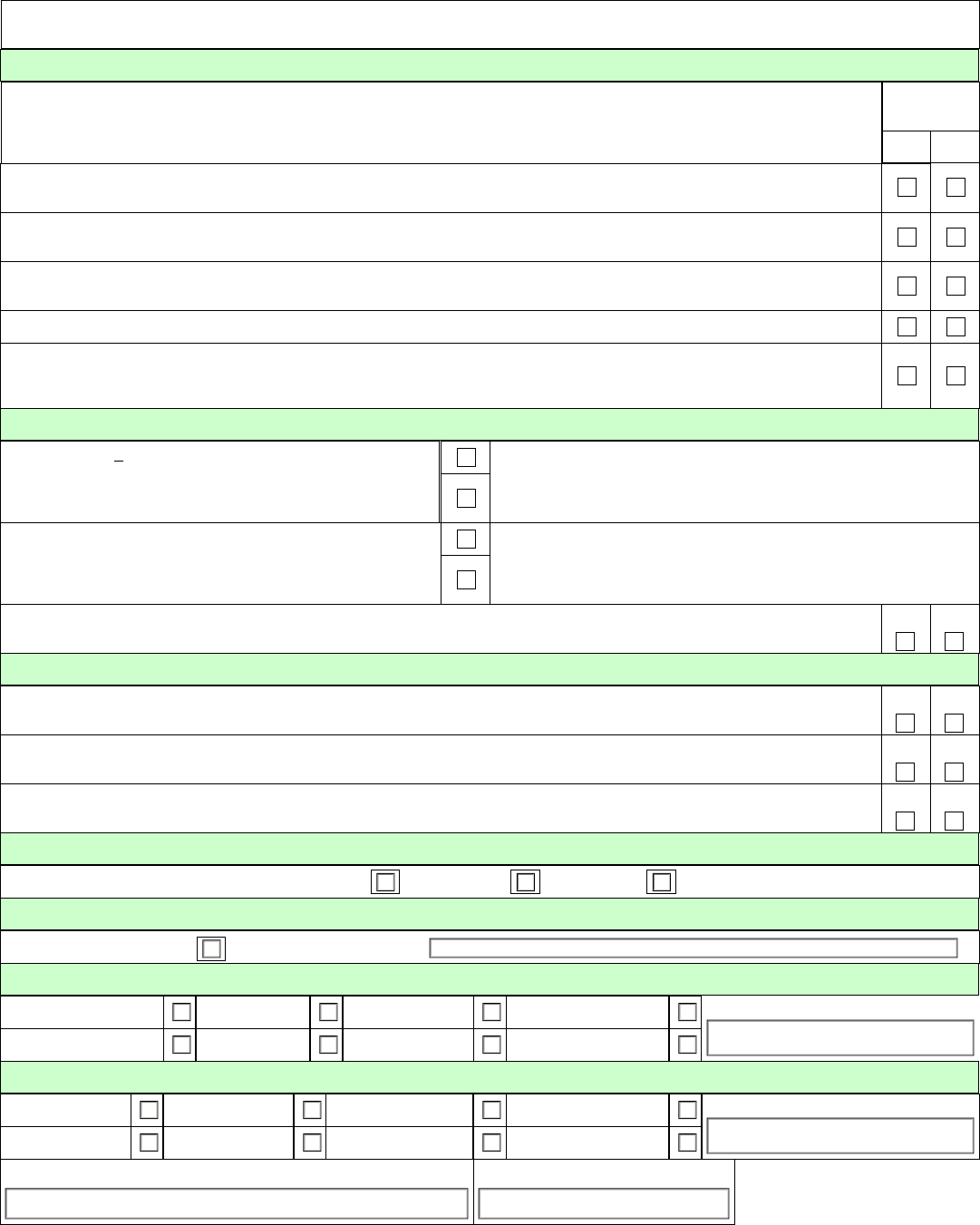
20. Goals of Care (check all that apply)
20.1 Rehabilitation (improved function)
20.2 Skilled nursing care (e.g., manage wounds,
medical devices, catheters, ostomy)
20.3 Monitoring/supervision to avoid clinical
complications
20.4 Improve compliance with medications/
treatments
21.17 Other (specify)
VA Geriatrics and Extended Care (GEC) Referral con't
21. Referring to which program? (Check all that apply)
20.5 Patient/Family Education
20.6 Respite (temporary relief for caregiver)
20.7 Palliative/End of Life Care
20.8 Reduce hospitalizations and/or ER visits
20.9 Supervised/supportive living situation
20.10 Behavior Stabilization
21.1 Skilled care in home
21.2 Home Based Primary Care
(HBPC)
21.3 ADL assistance (personal
care) in home
21.4 Chore Services (homemaker)
in home
21.5 Adult Day Health Care
21.6 Residential care (supervised
living)
21.7 Assisted Living
21.8 Domiciliary care
21.9 Short-term nursing home care
(subacute care, rehab,
etc)
21.10 Long-term nursing home care
21.11 Outpatient Respite care
21.12 Inpatient Respite care
21.13 Specialized Dementia or
Geropsych Care
21.14 Inpatient palliative/hospice care
(in NHCU)
21.15 Outpatient Palliative/ hospice
care (in home)
21.16 All inclusive care or PACE
program
22. Estimated Duration of Care
22.1 1 week 22.2 2-3 weeks 22.3 One month 22.4 2-3 months 22.5 4-6 months 22.6 Indefinite
Comments. (Any additional information that may be helpful to the referral program)
PATIENT'S LAST NAME, FIRST NAME, MIDDLE INITIAL SOCIAL SECURITY NO.
MAY 2006
VA FORM
10-0415
Page 4 of 5
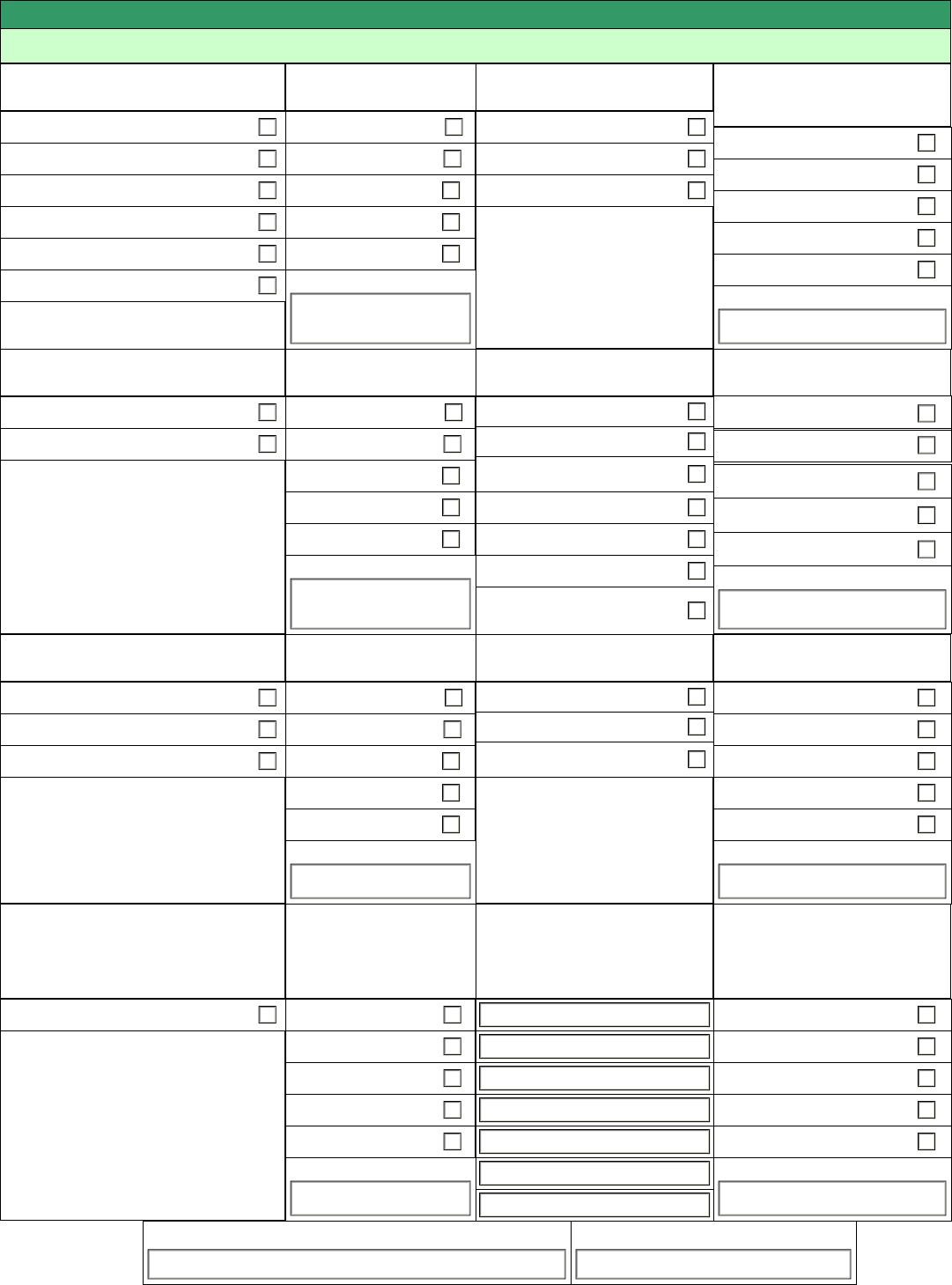
This Section for Administrative Use Only Use This Section Referral is processing (Check all that apply)
23. Where was the patient referred?
Home Care
Funding Sources for
Home Care
Structured Living Situation
Funding Sources for
Structured Living Situation
Community Skilled Home Health Care
VA
Personal Care Home
VA Home-Based Primary Care
Homemaker/Home Health Aide
VA Bowel and Bladder
Adult Day Health Care
VA In-home Respite
Medicare
Medicaid
Other insurance
Private Pay
Other (specify)
VA
Medicare
Medicaid
Other insurance
Private Pay
Community Residential Care
Assisted Living
Other (specify)
Domiciliary
Funding Sources for
Domiciliary
Nursing Home Care
Funding Sources for
Nursing Home Care
VA Domiciliary
VA
VA NHCU (Rehab)
State Home Domiciliary
Medicare
Medicaid
Other insurance
Private Pay
Other (specify)
VA
Medicare
Medicaid
Other insurance
Private Pay
VA NHCU (Long-term care)
VA NHCU (subacute care)
Other (specify)
VA NHCU (respite)
State Veterans nursing home
Community nursing home
VA NHCU (Hospice)
Hospice Care
Funding Sources for
Hospice Care
Geriatric Services
Funding Sources for
Geriatric Services
VA NHCU (Hospice) VA
GEM Clinic
VA Outpatient hospice Medicare
Medicaid
Other insurance
Private Pay
Other (specify)
VA
Medicare
Medicaid
Other insurance
Private Pay
Geriatric Primary Care Clinics
VA GEM inpatient unit
Other (specify)
Community hospice
Care Coordination/Home
Telehealth
Funding Sources for
Care Coordination/
Home Telehealth
OTHER (specify)
Funding Sources for
OtherServices
Care Coordination/Home Telehealth VA
Medicare
Medicaid
Other insurance
Private Pay
Other (specify)
VA
Medicare
Medicaid
Other insurance
Private Pay
Other (specify)
PATIENT'S LAST NAME, FIRST NAME, MIDDLE INTIAL SOCIAL SECURITY NO.
MAY 2006
VA FORM
10-0415
Page 5 of 5



