Fillable Printable 57.150 Ltacfacsurv Blank
Fillable Printable 57.150 Ltacfacsurv Blank
57.150 Ltacfacsurv Blank
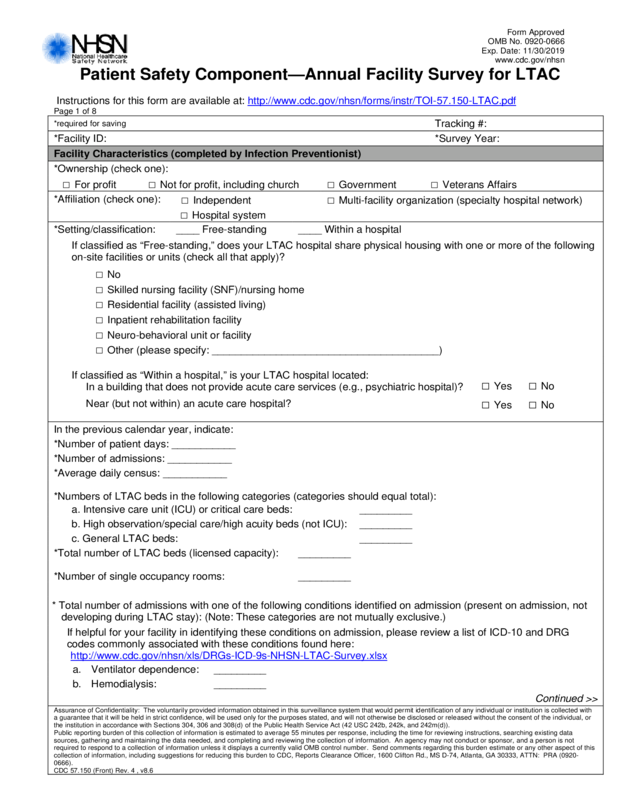
Form Approved
OMB No. 0920-0666
Exp. Date: 11/30/2019
www.cdc.gov/nhsn
Patient Safety Compo nent—Annual Facility Survey for LTAC
Instructions for thi s f orm are available at: http://www.cdc.gov/nhsn/forms/instr/TOI-57.150-LTAC.pdf
Page 1 of 8
*required for saving
Tracking #:
*Facility ID: *Survey Year:
Facility Characteristics (compl eted by I nfection Preventionist)
*Ownership (che ck one):
□ For profit □ Not for profit, including church □ Government □ Veterans Affairs
*Affiliation (check one):
□ Independent □ Multi-facility organization (specialty hospital network)
□ Hospital system
*Setting/classification: ____ Free-standing ____ Within a hospital
If classif ied as “Free-standing, ” does your LTAC hos pi t al share physical housing with one or more of the fol l owing
on-site facilities or units (check all that apply)?
□ No
□ Skilled nursing facility (SNF)/nursing home
□ Residential facility (assisted living)
□ Inpatient rehabilitation facility
□ Neuro-behavioral unit or facili t y
□ Other (please specify: _________ ___ ________ ___ ____ ____ _______ _)
If classified as “ Within a hospital,” is you r LTAC hospital locate d:
In a building that does not prov ide acute care services (e.g., psychi at ri c hospital)?
□ Yes □ No
Near (but not within) an acute care hospital?
□ Yes □ No
In the previous calendar year, indicate:
*Number of patient days: ___________
*Number of admissions: ___________
*Average daily cens us: ___________
*Numbers of LTAC beds in the following categories (categories should equal total):
a. Intensive care unit (ICU) or critical care beds: _________
b. High observat i on/special care/high a cuity beds (not ICU): _________
c. General LTAC beds: _________
*Total number of LT AC beds (licensed capacity): _________
*Number of single occ upancy rooms: _________
* Total number of admissions with one of the following conditi ons identified on admission (present on adm ission, not
developing during L T A C stay): (Note: These categories are not mutually exclusive. )
If helpful for your facil ity in identifying these conditions on adm ission, please rev i ew a list of ICD-10 and DRG
codes commonly as sociated with these conditions found here:
http://www.cdc.gov/nhsn/xls/DRGs-ICD-9s-NHSN-LTAC-Survey.xlsx
a. Ventilator dependence: _________
b. Hemodialysis: _________
Continued >>
Assurance of Confidentiality: The voluntarily provided information obtained in this surveillance system that would permit identification of any individual or institution is collected with
a guarantee that it will be held in strict confidence, will be used only for the purposes stated, and will not otherwise be disclosed or released without the consent of the individual, or
the institution in accordance with Sections 304, 306 and 308(d) of the Public Health Service Act (42 USC 242b, 242k, and 242m(d)).
Public reporting burden of this collection of information is estimated to average 55 minutes per response, including the time for reviewing instructions, searching existing data
sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not
required to respond to a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estima te or any other aspect of this
collection of information, including suggestions for reducing this burden to CDC, Reports Clearance Officer, 1600 Clifton Rd., MS D-74, Atlanta, GA 30333, ATTN: PRA (0920-
0666).
CDC 57.150 (Front) Rev. 4 , v8.6
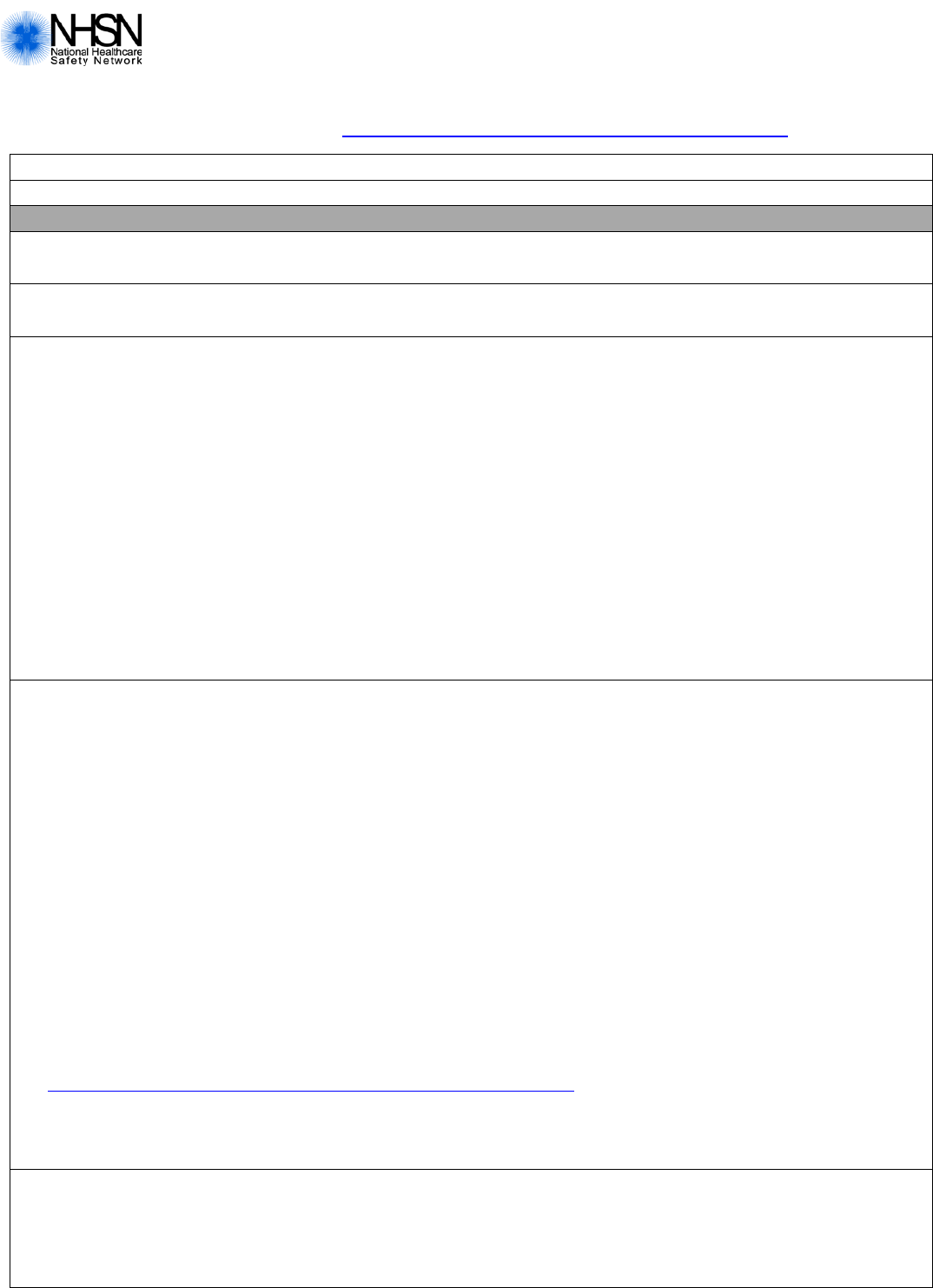
Form Approved
OMB No. 0920-0666
Exp. Date: 11/30/2019
www.cdc.gov/nhsn
CDC 57.150 (Back), Rev. 4, v8.6
Patient Safety Component—Annual Facility Survey for LTAC
Page 2 of 8
Facility Microbiology Laboratory Practices (completed with input from Microbiology Laboratory Lead)
*1. Does your facilit y have its own on-site laboratory that performs ant i mi crobial susceptibility testing?
□ Yes □ No
If No, where is your fa cil i t y’s antimicrobi al susceptibility testing performed? (check one)
□ Affiliated medical center □ Commercial referral l aboratory
□ Other local/regional, non-affiliated
reference laboratory
*2. For the following organisms plea se indicate which methods are used for:
(1) primary suscepti bi l ity testing and
(2) secondary, supplemental, or confi rmatory testing (if performed).
If your laboratory does not perform susceptibility testi ng, please indicate the methods used at the outside
laboratory.
Please use th e testing codes listed below the tabl e.
Pathogen (1) Primary (2) Secondary Comments
Staphylococcus aureus
_______________ ______________ ______________
Enterobacteriaceae _______________ ______________ ______________
1 = Kirby-Bauer disk diffus i on 5.1 = MicroScan walkaway rapid 10 = E test
2 = Vitek (Lega cy) 5.2 = MicroScan walkaway conventional 12 = Vancomycin agar screen (BH I + vancomycin)
2.1 = Vitek 2 5.3 = MicroScan auto or touc hscan 13 = Other (describe in Comments s ec tion)
3.1 = BD Phoenix 6 = Other micro-broth dilution method
4 = Sensititre 7 = Agar dilution method
*3. Has the laboratory im plemented the revised cephalosporin and monobactam
breakpoints for Enterobacteriaceae recommended by CLSI as of 2010?
□ Yes □ No
*4. Has the laboratory im plemented the revised carbapenem b reakpoints for
Enterobacteriaceae recommended by CLSI as of 2010?
□ Yes □ No
*5. Does the laboratory perform a special test for presence of carbapenemase?
□ Yes □ No
If Yes, please indicate what is done if car bapenemase production is detected: (check one)
□ Change susceptibl e carbapenem results to resistant
□ Report carbape nem M IC results with out an interpretati on
□ No changes are made i n the interpretation of carb apenems, the test is used for epidemiological or
infection control purpose s
If Yes, which test is routinely performed to detect carbapen em ase: (check all that apply)
□ PCR □ MBL screen
□ Modified Hodge Test □ Carba NP
□ E test □ Other (specify): _________________
Continued >>
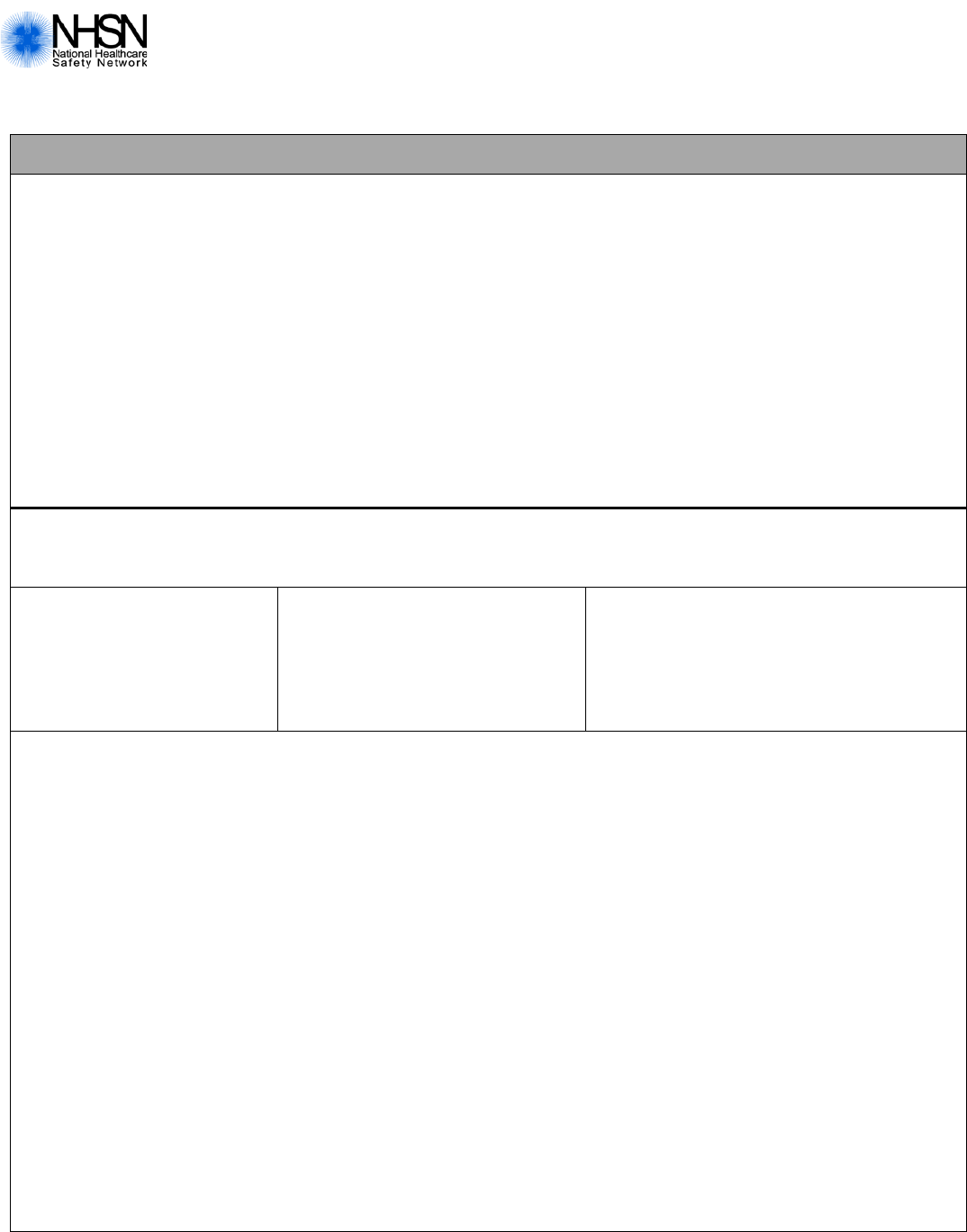
Form Approved
OMB No. 0920-0666
Exp. Date: 11/30/2019
www.cdc.gov/nhsn
CDC 57.150 (Back), Rev. 4, v8.6
Patient Safety Component—Annual Facility Survey for LTAC
Page 3 of 8
Facility Microbiology Laboratory Practices (continued)
*6. Does the laboratory perform colistin or polymyxin B suscepti bi l ity testing for drug-resistant gram
negative bacilli ?
□ Yes □ No
If Yes, please indicate m ethods: (check all that apply)
□ Vitek (Legacy) □ MicroScan walkaw ay rapid □ Agar dilution method
□ Vitek 2 □ MicroScan walkaw ay conventional □ E test
□ BD Phoenix □ MicroScan auto or touchscan □ Other (specify): _____________________
□ Sensititre □ Other micro-broth dil ution method
*7. Does your facilit y have its own laboratory that performs ant i f ungal susceptibility testing for Candida species?
□ Yes □ No
If No, where is your fa cil i t y’s antifungal sus cept i bil i ty testing perfo rmed? (check one)
□ Affiliated medical center □ Commercial referral l aboratory
□ Other local/regional, non-affiliated reference labo ratory □ Not offered by my facility
8. If antifungal susceptibility testi ng i s performed at your facility or an outside laboratory, what methods are used?
(check all that apply)
□ Broth macrodilution □ Broth microdilution □ YeastOne colorimetri c microdil ution □ E test
□ Vitek 2 card □ Disk diffusion □ Other (specify): ________________
*9. Is antifungal susceptibility testing performed automatically/reflex ively without needing a specific orde r or request for
susceptibility testing from the clini cian for the below Candida species when cultured from normall y sterile body
sites (such as blood)?
Candida albicans:
□ Yes □ No
If Yes, what antifungal drugs are tested automatically/refl exively? (check all that apply)
□ Fluconazole □ Voriconazole □ Anidulafungin/Caspofungin/Micafungin
Candida glabrata:
□ Yes □ No
If Yes, what antifungal drugs are tested aut om atically/reflexi vely? (check all that apply)
□ Fluconazole □ Voriconazole □ Anidulafungin/Caspofungin/Micafungin
Candida parapsilosis:
□ Yes □ No
If Yes, what antifungal drugs are tested automatically/refl exively? (check all that apply)
□ Fluconazole □ Voriconazole □ Anidulafungin/Caspofungin/Micafungin
Other Candida species:
□ Yes □ No
If Yes, what antifungal drugs are tested automatically/refl exively? (check all that apply)
□ Fluconazole □ Voriconazole □ Anidulafungin/Caspofungin/Micafungin
□ Automatic testing is not performed for any Candida species
Continued >>

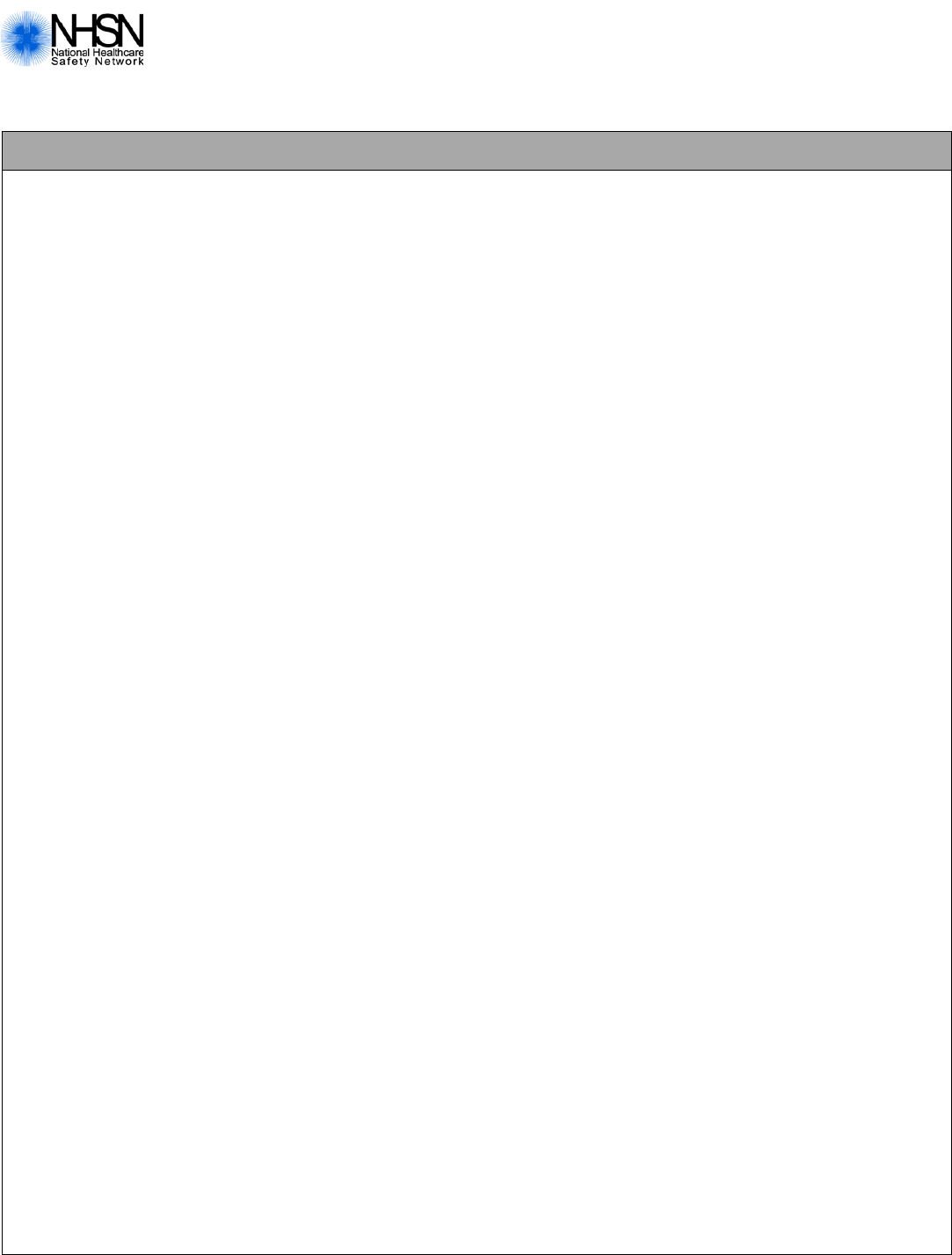
Form Approved
OMB No. 0920-0666
Exp. Date: 11/30/2019
www.cdc.gov/nhsn
CDC 57.150 (Back), Rev. 4, v8.6
Patient Safety Component—Annual Facility Survey for LTAC
Page 4 of 8
Facility Microbiology Laboratory Practices (continued)
*10. What is the primary testing method f or C. difficile used most often by your facility’s laboratory or the outside
laboratory where y our facility’s t est i ng i s performed? (check one)
□ Enzyme immunoassay (EIA) for toxin
□ Cell cytotoxi cit y neutralization assay
□ Nucleic acid amplification test (NAAT) (e.g., PCR, LAMP)
□ NAAT plus EIA, if NAAT positive (2-step algorithm)
□ Glutamate dehydrogenase (GDH) a ntigen plus EIA for t oxin (2-step algorithm)
□ GDH plus NAAT (2-step algorithm)
□ GDH plus EIA for toxin, followed by NAAT for disc repant results
□ Toxigenic culture (C. difficile culture fol lowed by detection of toxins)
□ Other (specify): ______________________
(“Other” should not be used to name specif i c laboratories, refer ence laboratories, or t he brand names of C.
difficile tests; m ost m ethods can be categorized accurately by selecting f rom the options provided. P l ease ask
your laboratory or conduct a search for furt her guidance on sele ct i ng the correct option t o report.)
*11. Does your facility produce an antib iogram (i.e., cumulative antimicrobial su sceptibility report)?
□ Yes □ No
If Yes, is the antibiogram produced at least annually?
□ Yes □ No
If Yes, are data stratified by hospit al l ocation?
□ Yes □ No
If No, please identify any obst acle(s) to producing an antibiogram. (Check all that apply)
□ The laboratory data are difficult to acc ess
□ Limited or no information technology tool for data analysis
□ Limited personnel t i m e for data analysis
□ Limited personnel skills for data analysis
□ Limited interest i n an antibiogram fro m staff who prescribe antibiotics
□ Our institution does not have enough isolat es of any or most species (i.e., < 30 isolates per specie s) t o
produce an antibiogram
□ Other (please specify ): ________ ___ ____ _______ ____ ____ _______ ____ __
Infection Control Practices
(completed with input from Hospital Epidemiologist and/or Quali ty Improvement Coordinator)
*12. . Number or fraction of infection preventionists (IPs) in facility: _______
a. Total hours per week performing survei l l ance: _______
b. Total hours per week f or infection control acti vities other than surveillance: _______
*13. Number or fra ct ion of full-time employees (FTEs) for a designated hospital epidemiologist
(or equivalent role) aff iliate d with your facility:
_______
Continued >>
Form Approved
OMB No. 0920-0666
Exp. Date: 11/30/2019
www.cdc.gov/nhsn
CDC 57.150 (Back), Rev. 4, v8.6
Patient Safety Component—Annual Facility Survey for LTAC
Page 5 of 8
Infection Control Practices
(completed with input from Hospital Epidemiologist and/or Quali ty Improvement Coordinator)
*14. Is it a policy in your facility that patients infected or coloni zed with MRSA are routinel y plac ed in co ntact precauti ons
while these patients are in your facility? (ch eck one)
□ Yes, all infected o r colonized patients
□ Yes, only all infected pat i ents
□ Yes, only those with certain characterist i cs that make them hig h-risk for transmission (e.g., wounds, diarrhea,
presence of an indwel l ing device)
□ Yes, only those admitt ed to high-risk settings (e.g., ICU)
□ No
□ Not applicable: my facility never admits these patients
*15. Is it a policy in your facility that patients infected or coloni zed with VRE are routinely placed in contact precautions
while these patients are in your facility? (ch eck one)
□ Yes, all infected or colonized patients
□ Yes, only all infected pat i ents
□ Yes, only those with certain characterist i cs that make them hig h-risk for transmission (e.g., wounds, diarrhea,
presence of an indwel l ing device)
□ Yes, only those admitt ed to high-risk settings (e.g., ICU)
□ No
□ Not applicable: my facility never admits these patients
*16. Is it a policy in your facility that patients infected or coloni zed with CRE (regardless of confirmatory t esting for
carbapenemase pr oduction) are routinely placed in contact precautions while these patients are in your f acil ity?
(check one)
□ Yes, all infected o r colonized patients
□ Yes, only all infected pat i ents
□ Yes, only those with certain characterist i cs that make them hig h-risk for transmission (e.g., wounds, di arrhea,
presence of an indwel l ing device)
□ Yes, only those admitt ed to high-risk settings (e.g., ICU)
□ No
□ Not applicable: my facility never admits these patients
*17. Is it a policy in y our facility that patients infected or colonized with suspected or confirmed ESB L -producing or
extended spectrum cephal osporin re sist ant Enterob a cteria ceae ar e routinely placed in contact precautions while
these patients are in y our facility? (check one)
□ Yes, all infected o r colonized patients
□ Yes, only all infected pat i ents
□ Yes, only those with certain characterist i cs that make them hig h-risk for transmission (e.g., wounds, diarrhea,
presence of an indwel l ing device)
□ Yes, only those admitted to high-risk settings (e.g., ICU)
□ No
□ Not applicable: my facility never admits these patients
Continued >>
Form Approved
OMB No. 0920-0666
Exp. Date: 11/30/2019
www.cdc.gov/nhsn
CDC 57.150 (Back), Rev. 4, v8.6
Patient Safety Component—Annual Facility Survey for LTAC
Page 6 of 8
Infection Control Practices
(completed with input from Hospital Epidemiologist and/or Quali ty Improvement Coordinator)
*18. Does the facility routinely perform screening testing (culture or non-culture) for CRE?
□ Yes □ No
If Yes, in which situat i ons does the facilit y routinely perform s cre ening testing for C RE ? (check all that apply )
□ Surveillance testing at admis sion for all patients
□ Surveillance testing of epidemiologically-linked pati ents of newly identifi ed CRE patients (e.g., roommates)
□ Surveillance testing at admis sion of high-risk patients (e.g., admitted from L T AC or LTCF)
□ Surveillance testing at admis sion of patients admitted to high-risk settings (e.g. ICU)
□ Other (please specify): ________ _________
*19. Does the facility routinely perform screening testi ng (c ul t ure or non-culture) for MRSA?
□ Yes □ No
If yes, in which situations does the fa cil ity routinely perform screening testi ng for MRSA? (check all that apply)
□ Surveillance testing at admis sion for all patients
□ Surveillance testing at admis sion of high-risk patients (e.g., admitted from L T AC or LTCF)
□ Surveillance testing at admis sion of patients admitted to high-risk settings (e.g. ICU)
□ Surveillance testing of pre-operat i ve patients to prevent surgical site i nfections
□ Other (please specify): ________ _________
*20. Does the f acil ity routinely use chlor hexidine bathing on any patient to prevent i nfection or transmission of MDROs
at your facility? (Note: this does not include the u se of such bathing in pre-operative pati ent s to prevent SSIs)
□ Yes □ No
*21. Does the facili t y routinely use a com bi nation of topical chl orhexidine AND intranasal mupirocin (or equiv alent
agent) on any pat i ents to prevent inf ecti on or transmission of M RS A at your facility? (Note: t his does not include
the use of these agents in pre-operative surgical patients or dialysis patients)
□ Yes □ No
*22. Among patients with an MDRO admitted to your facility from another healt hcare facility, pl ease estimate how often
your facility receives information from the transferring facility abou t the patient’s MDR O st atus?
□ All the time
□ More than half of the time
□ About half of the time
□ Less than half of the time
□ None of the time
□ Not applicable: my f acil i t y does not receive transferred patients with a known MDRO
Continued >>
Form Approved
OMB No. 0920-0666
Exp. Date: 11/30/2019
www.cdc.gov/nhsn
CDC 57.150 (Back), Rev. 4, v8.6
Patient Safety Component—Annual Facility Survey for LTAC
Page 7 of 8
Antibiotic Stewardship Practices
(completed with input from Physician and Pharmacist Stewardship Champions)
*23. Does your facilit y have a written statem ent of support from leadership that supports efforts to improve antibiotic use
(antibiotic stewar dship)?
□ Yes □ No
*24. Is there a leader resp onsible for stewardship activities at your facility?
□ Yes □ No
If Yes, what is the position of this leader: (check one )
□ Physician □ Co-led by both Pharmacist and Physician
□ Pharmacist □ Other (please specify): _______________________
*25. Is there at least one pharmacist res ponsible for improvin g antibiotic use at y our f acil ity?
□ Yes □ No
*26. Does your facili ty provide any sala ry support for dedicated t i m e for antibiotic steward ship leadership activities?
□ Yes □ No
*27. Does your facili ty have a policy that requires prescribers to document an i ndication for all antibiotics in the m edi cal
record or during order entry?
□ Yes □ No
If Yes, has adherence to the policy to document an indication been monit ored?
□ Yes □ No
*28. Does your facili ty have facility-sp ecific treatment rec om mendations, based on national guidelines and local
susceptibility, t o assi st with antibiotic selection for common clinical conditio ns?
□ Yes □ No
If Yes, has adherence to f acili ty-specific treatment recommendations bee n m oni tored?
□ Yes □ No
*29. Is there a formal procedure for all clini cians to review the app ropriateness of all antibiotics at or after 48 hours from
the initial orders (e.g. antibiotic time out)?
□ Yes □ No
*30. Do any specified antibiotic agent s need to be approved by a physician or pharmacist prior to dispen sing at your
facility?
□ Yes □ No
Continued >>
Form Approved
OMB No. 0920-0666
Exp. Date: 11/30/2019
www.cdc.gov/nhsn
CDC 57.150 (Back), Rev. 4, v8.6
Patient Safety Component—Annual Facility Survey for LTAC
Page 8 of 8
Antibiotic Stewardship Practices (continued)
*31. Does a physici an or pharmacist rev iew courses of therapy f or specified antibiotic agents and communicate results
with prescribers at your facility?
□ Yes □ No
If Yes, what type of feedback is provided to pres cribers? (check all t hat apply)
□ Feedback on antimic robial route and/or dosage
□ Feedback on the selection of antimicr obi al therapy and/or durat i on of therapy
□ Other (please specify) : ___________________________________________
*32. Does your facility monitor antibiotic use (consumpt ion) at the unit, service, and/or facility wide?
□ Yes □ No
If Yes, by which metrics? ( Check all that apply)
□ Days of Therapy (DOT) □ Purchasing Data
□ Defined Daily Dose (D DD ) □ Other (please specify): ________________________
If Yes, are facility- and/or unit- or service-specific report s on antibiotic use shared with prescribers?
□ Yes □ No
*33. Has your facility provi ded education to clinicians and other relevant staff on improving antibiotic use?
□ Yes □ No



