Fillable Printable Appendix F Postpartum Depression
Fillable Printable Appendix F Postpartum Depression
Appendix F Postpartum Depression
T
OOL KIT
FOR THE
M
ANAGEMENT OF
A
DULT
P
OSTPARTUM
D
EPRESSION
This tool kit was developed by the AHCCCS Tool Kit Workgroup in collaboration with Acute Health Plans and ADHS/DBHS (January, 2008
through January, 2009). This tool kit is only a resource and may not apply to all patients and all clinical situations. It is not intended to replace
clinical judgment.
Initial Effective Date: 05/01/2009 Revision Date: 05/01/2011, 12/01/09
TOOL KIT FOR THE MANAGE MENT OF
A
DULT POSTPARTUM DEPRESSION
The clinical tool kit is intended to assist the PCP in assessing the postpartum needs of women
regarding depression and decisions regarding health care services provided by the PCP or
subsequent referral to the Regional Behavioral Health Authority (RBHA) if clinically indicated.
Tools include:
• The decision making algorithm for depression
• Edinburgh Postnatal Depression Scale with accompanying scoring instructions
• The Postpartum Safety Screening
• The list of medications universally available through AHCCCS Health Plans and the
RBHA.
** CLINICIAN NOTE:
In the assessment of postpartum depression, the clinician should review for the possible
existence of psychotic symptoms since 1/1000 women may suffer with psychotic symptoms a
part of this mood disorder. These symptoms include:
1) Delusions
2) Hallucinations
3) Disorganized Speech
4) Inappropriate Behavior
These severe symptoms can last for one day or up to a month. In some cases, the symptoms of
psychosis may accompany periods of restlessness or agitation. Psychiatric consultation and/or
emergency referral should occur.
** A RBHA consultation is available at any time.
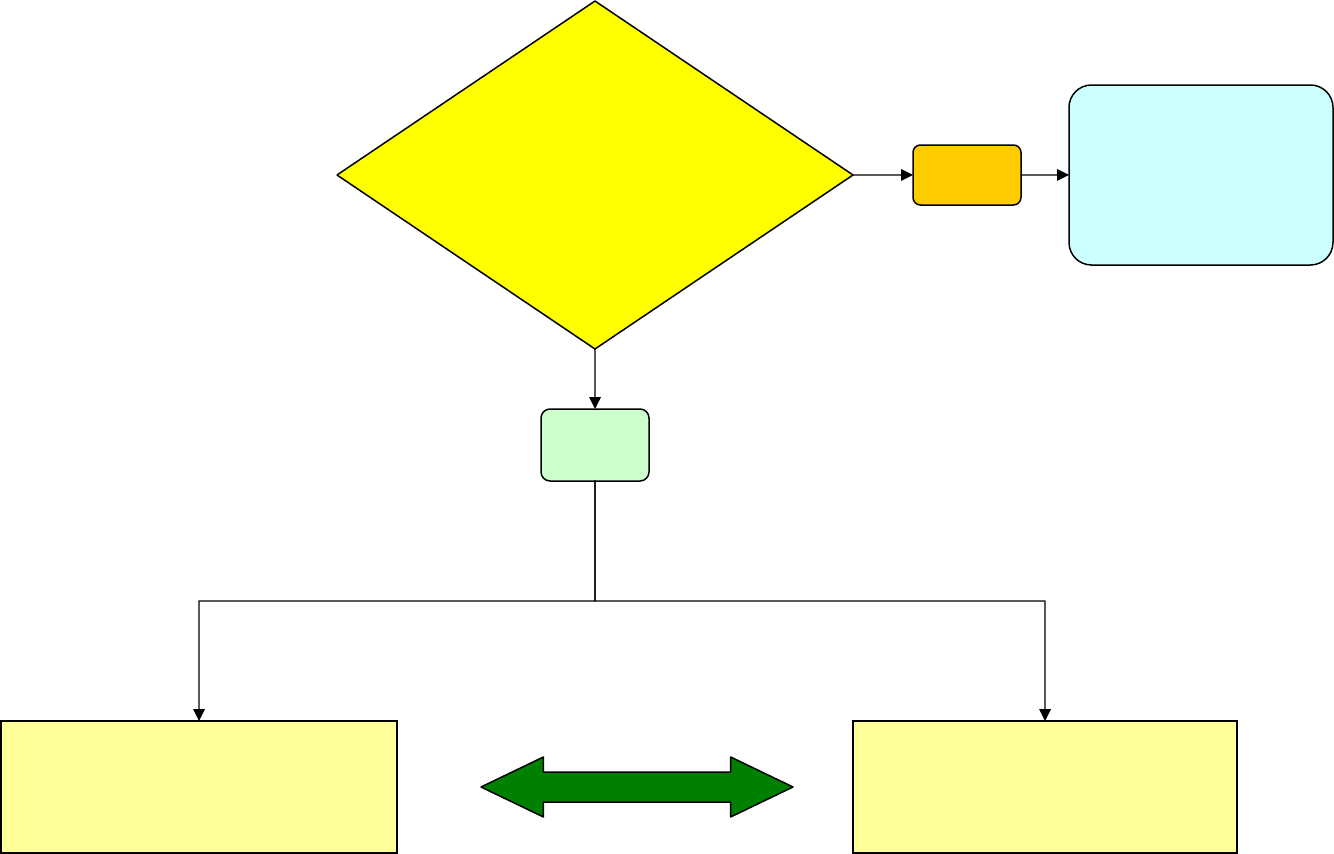
Depression
Danger to Self
or
Others
Refer to
RBHA
Treatment
By PCP
Refer to
RBHA
NO
YES
*Sole usage of Algorithms is not a substitute for a comprehensive clinical assessment
EdinburghPostna talDepressionScale
1
(EPDS)
Name: ______________________________ Address: ___________________________
Your Date of Birth: ____________________ ___________________________
Baby’s Date of Birth: ___________________ Phone:
_________________________
As you are pregnant or have recently had a baby, we would like to know how you are feeling. Please check
the answer that comes closest to how you have feltINTHEPAST7DAYS, not just how you feel today.
Here is an example, already completed.
I have felt happy:
Yes, all the time
Yes, most of the time This would mean: “I have felt happy most of the time” during the past week.
No, not very often Please complete the other questions in the same way.
No, not at all
In the past 7 days:
1. I have been able to laugh and see the funny side of things *6. Things have been getting on top of me
As much as I always could Yes, most of the time I haven’t been able
Not quite so much now to cope at all
Definitely not so much now Yes, sometimes I haven’t been coping as well
Not at all as usual
No, most of the time I have copied quite well
2. I have looked forward with enjoyment to things No, I have been coping as well as ever
As much as I ever did
Rather less than I used to *7 I have been so unhappy that I have had difficulty sleeping
Definitely less than I used to Yes, most of the time
Hardly at all Yes, sometimes
Not very often
*3. I have blamed myself unnecessarily when things No, not at all
went wrong
Yes, most of the time *8 I have felt sad or miserable
Yes, some of the time Yes, most of the time
Not very often Yes, quite often
No, never Not very often
No, not at all
4. I have been anxious or worried for no good reason
No, not at all *9 I have been so unhappy that I have been crying
Hardly ever Yes, most of the time
Yes, sometimes Yes, quite often
Yes, very often Only occasionally
No, never
*5 I have felt scared or panicky for no very good reason
Yes, quite a lot *10 The thought of harming myself has occurred to me
Yes, sometimes Yes, quite often
No, not much Sometimes
No, not at all Hardly ever
Never
Administered/Reviewed by ________________________________ Date ______________________________
1
Source: Cox, J.L., Holden, J.M., and Sagovsky, R. 1987. Detection of postnatal depression: Development of the 10-item
Edinburgh Postnatal Depression Scale. BritishJournalofPsychiatry 150:782-786.
2
Source: K. L. Wisner, B. L. Parry, C. M. Piontek, Postpartum Depression N Engl J Med vol. 347, No 3, July 18, 2002,
194-199
Users may reproduce the scale without further permission providing they respect copyright by quoting the names of the
authors, the title and the source of the paper in all reproduced copies.
EdinburghPostnatalDepressionScale
1
(EPDS)
Postpartum depression is the most common complication of childbearing.
2
The 10-question Edinburgh
Postnatal Depression Scale (EPDS) is a valuable and efficient way of identifying patients at risk for “perinatal”
depression. The EPDS is easy to administer and has proven to be an effective screening tool.
Mothers who score above 13 are likely to be suffering from a depressive illness of varying severity. The EPDS
score should not override clinical judgment. A careful clinical assessment should be carried out to confirm the
diagnosis. The scale indicates how the mother has feltduringthepreviousweek. In doubtful cases it may
be useful to repeat the tool after 2 weeks. The scale will not detect mothers with anxiety neuroses, phobias or
personality disorders.
Women with postpartum depression need not feel alone. They may find useful information on the web sites of
the National Women’s Health Information Center <www.4women.gov> and from groups such as Postpartum
Support International <www.chss.iup.edu/postpartum> and Depression after Delivery
<www.depressionafterdelivery.com>.
SCORING
QUESTIONS1,2,&4( withoutan*)
Are scored 0, 1, 2 or 3 with top box scored as 0 and the bottom box scored as 3.
QUESTIONS3,510(markedwit han*)
Are reverse scored, with the top box scored as a 3 and the bottom box scored as 0.
Maximum score: 30
Possible Depression: 10 or greater
Always look at item 10 (suicidal thoughts)
Users may reproduce the scale without further permission, providing they respect copyright by quoting the
names of the authors, the title, and the source of the paper in all reproduced copies.
Instructionsfo rusingt heEdinburghPostnatalDepre ssionSca le:
1. The mother is asked to check the response that comes closest to how she has been feeling
in the previous 7 days.
2. All the items must be completed.
3. Care should be taken to avoid the possibility of the mother discussing her answers with
others. (Answers come from the mother or pregnant woman.)
4. The mother should complete the scale herself, unless she has limited English or has difficulty
with reading.
1
Source: Cox, J.L., Holden, J.M., and Sagovsky, R. 1987. Detection of postnatal depression: Development of the 10-item
Edinburgh Postnatal Depression Scale. BritishJournalofPsychiatry 150:782-786.
2
Source: K. L. Wisner, B. L. Parry, C. M. Piontek, Postpartum Depression N Engl J Med vol. 347, No 3, July 18, 2002,
194-199
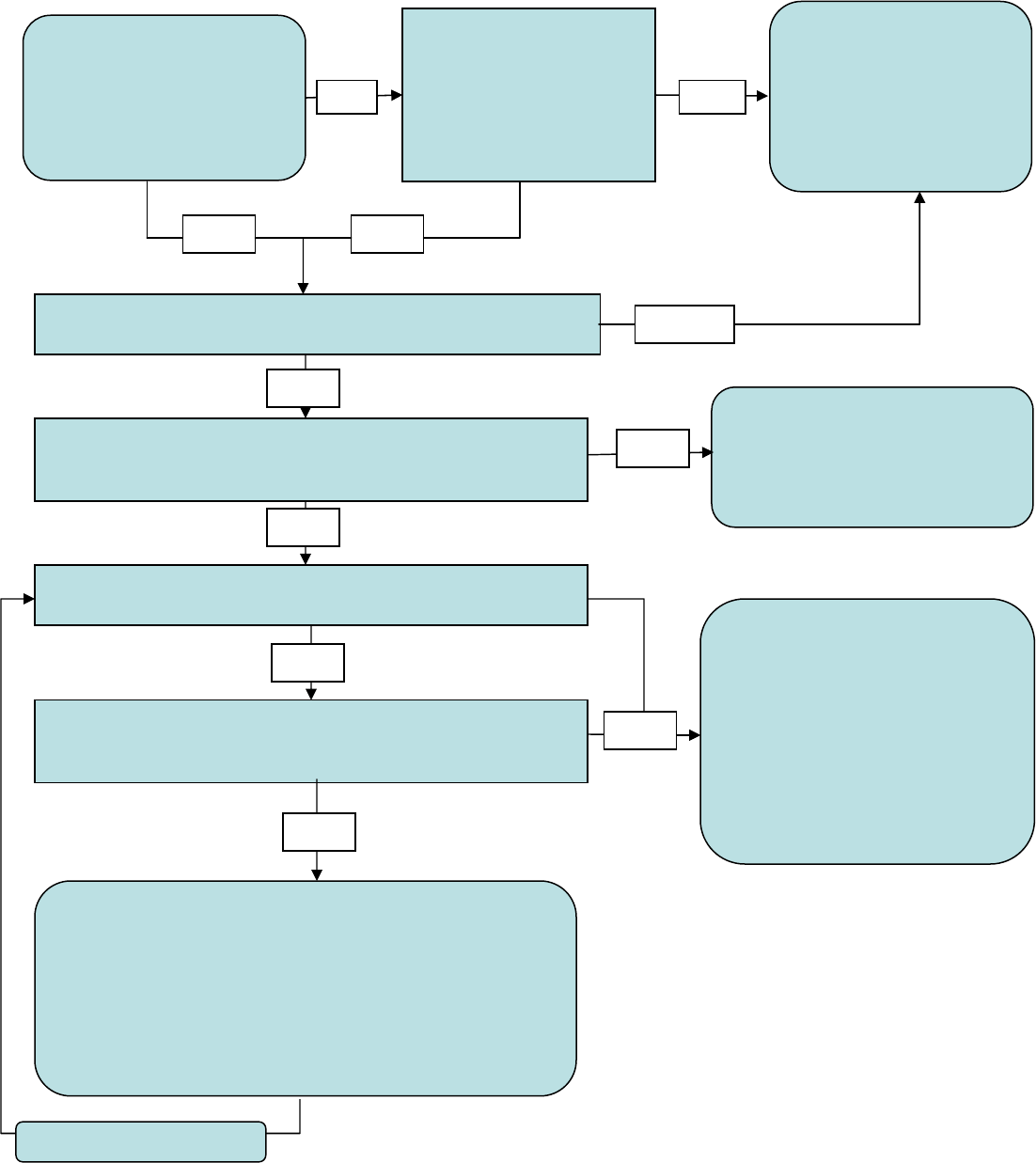
Mother is exhibitin g bizarre
or unusual behavior or
beliefs (e. g. e xtrem es o f
mood, especially elation,
seeming lack of sleep;
strange ideas about the
baby)
The PCP, Mother and/or her
family is concerned about
the new mother’s mood or
behaviors or the new mother
has a score of 10 or greater
on the Edinburgh (EPDS)
Is she exhibiting suicidal or infanticidal thoughts or thoughts of
wanting to run away with infant?
Do the symptoms impair the new mother’s ability to care for
herself, the infant, other children (e.g. she is unable to out of
bed)?
yes
yes yes
Have symptoms (mood or behavior changes) been present for
two or more weeks?
Have symptoms resulted in significant disruptions to appetite or
sleep pattern, or physical symptoms such as racing heart,
shortness of breath, dizziness, or GI upset
Assess and refer to
Emergency Department –
If no other responsible
parent/caregiver is
availabl e; refer to Child
Protective Services
( 1-888-767-2445)
1)Refer pat ient to RBHA provider
2)Request updates daily from the
co-parent, partner, family
member until the person is
evalua te d by th e RBHA Provid er
1)Refer to community supports, including new homes
groups or post-partum groups in the area
2)Educate the parent on Arizona’s *Safe Haven Law
3)Evaluate chronic stressors (e.g. inadequate or unsafe
housing, social isolation) and refer to social services or to
the RBHA for psychotherapy
4)Provide the local RBHAs crisis helpline
5)Follow up as clinically indicated
1) Evaluate or refer to the RBHA
provider
2 )If treating, follow-up as
clinically appropriate to assess
the effectiveness of treatment
3) After two weeks, if there is n o
evidence of symptom reduction,
refer to the RBHA provider or the
Emergency Department, if
appropriate
yes
no
yes
Postpartum Safety
Screening
no
Continue to Evaluate
*Safe Haven Law
According to Arizona State Law you can give
your baby to a Safe Haven provider without fear of
being arrested or anyone trying to identify or find you
as long as the baby is less than 3 days old and is left
with a staff member at a fire station or hospital, the
baby has not been physically harmed and you do
do not plan to return for the baby at a later time.
(Arizona Revised Statute-13-3623)
no
no
no
no
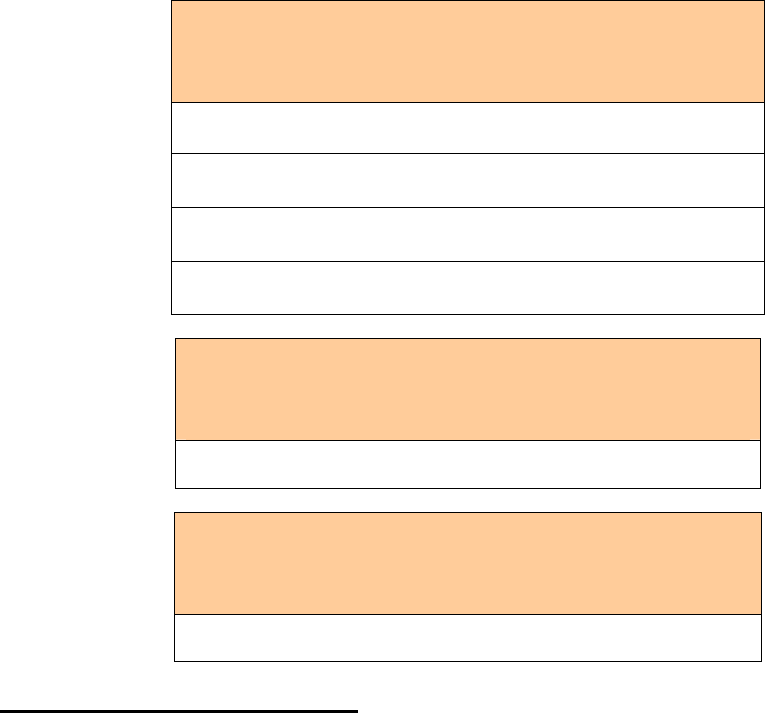
P
OSTPARTUM DEPRESSION
UNIVERSALLY AVAILABLE MEDICATIONS THROUGH
AHCCCS HEALTH PLANS AND RBHA PROVIDERS*
SELECTIVE SEROTONIN
REUPTAK E INHIBITOR
Fluoxetine (Prozac)
Citalopram (Celexa)
Paroxetine (Paxil)
Sertraline (Zoloft)
SEROTONIN NOREPINEPHRINE
REUPTAKE INHIBITOR
Venlafaxine (Effexor)
NOREPINEPHRINE DOPAMINE
REUPTAKE INHIBITOR
Bupropion (Wellbutrin)
Note for Use by Lactating Women:
• For lactating mothers who have no history of antidepressant treatment, an antidepressant, such as paroxetine or
sertraline should be first choice due to the evidence that these drugs produce very low drug levels in breast milk
and infant serum and have few side effects.
• For lactating mothers who have been successfully treated with a particular SSRI, TCA, or SNRI in the past, the
data and information for the previous specific antidepressant should be reviewed and carefully considered for
first-line treatment if there are no contraindications.
• There are insufficient reports to support the use of venlafaxine, bupropion and duloxetine, however if a member
was stable on one of these medications previously then the specific medication should be evaluated and
considered for first-line treatment.
• Strategies to decrease infant exposure to the drug include administering the drug after feedings or pumping and
discarding breast milk obtained during expected peak infant serum levels.
*Refer to health plan for prior authorization requirements.
Initial Effective Date: 05/01/2009 Revision Date: 05/01/2011, 12/01/09



