Fillable Printable Claimsclues February2013
Fillable Printable Claimsclues February2013
Claimsclues February2013
CLAIMS CLUES
A Publication of the AHCCCS Claims Department
February 2013
INFORMATION FROM THE OFFICE OF THE INSPECTOR
GENERAL
The Arizona Health Care Cost Containment System (AHCCCS) Office of Inspector General has identified a number
of claims and/or encounters that are in violation of AHCCCS Rules and Policy related to “Rendering Providers”.
This communication should serve as notice that all claims and/or encounter s submitt ed MUST list the appropriate
rendering provider as defined below.
6.5.4 CMS- 1500 Provider Definitions
…Rendering Provider:
The rendering provider is the individual who provided the care to the client. In the case where a substitute provider
was used, that individual is considered the rendering provider.
An individual such as a lab technician or radiology technician who performs services in a support role is not
considered a rendering provider.
The AHCCCS Participating Provider Agreement #19 states that “No provider may bill with another provider’s ID
number, except in locum tenens situations”. [AHCCCS Administration will recognize locum tenens arrange ment s
restricted to the length of the locum tenens registration with the AMA. The locum tenens provider must submit claims
using the AHCCCS provider ID number of the physician for whom the locum tenens provider is substituting or
temporarily assisting.]
Additionally, the AHCCCS Fee for Service Provider Manual states that “Hospitals and clinics may not bill AHCCCS
Administration or its Contractors for physician and mid-level practitioner services using the hospital or clinic NPI
number. Physicians and mid-level practitioners must register with AHCCCS and bill for services under their individual
NPI numbers”.
As an example, the following scenario illustrates one of many possible inappropriate billing practices.
An AHCCCS member receives services from a mid-level practitioner, (physician assistants, registered nurse
practitioners, certified nurse-midwives, certified registered nurse anesthetists (CRNA’s), surgical first assistants, and
affiliated practice dental hygienists.) following receipt of services, a claim or encounter is then submitted listing
another AHCCCS registered provider (typically a physician) as the rendering provider.
The Office of Inspector General will continue auditing claims and/or encounters to identify this improper activity which
may result in the denial of claims, recoupment of funds or the issuance of Civil Monetary Penalties.
CLAIM TIPS AND REMINDERS:
• When submitting a paper Fee for Service claim to AHCCCS providers MUST
indicate the claims “from dat e of service” and the “to date of service” in ord e r
for the claim to be processed properly in our claims system.
• Outlier claim records- please be sure to submit all records required for outlier
review. The easiest way to decide what to send is to review your IZ. If the
charge appears on the IZ, we will require records to substantiate that charge.
Frequently Medication Administration records are not submitted on outlier
claims.
PERM 2012 ERRORS
As part of our PERM corrective action plan, we are required by CMS to
find solutions for any errors or deficiencies that were cited against us
during the PERM audit. We thought that we would share with our
provi d ers the er rors and d eficiencies that were found d uring the recent
PERM audit. In some instances, referrals to the Office of the Inspector
General have been made regarding these errors o r audi ts have been
initiated. CMS will closely monitor these errors during future PERM audits
to see if they beco m e a trend .
Errors:
• Insufficient documentati on of services performed
o Provider billed for 99238 but did not have documentation
to supp o rt the service being p erformed.
• Wrong nu m ber of units billed
o Provider billed 90960 but could only provide
documentation for 2 of 4 services.
• Improper billing
o Provi der billed for serv ices never perfor m ed.
Deficiencies:
• Billing for Wrong Da te of Service

What ca n be learne d from the errors & defic iencies listed ab o ve?
• Providers must bill for services that are actually being performed.
Referrals to the Office of the Inspector Genera l will be made for
any potential fraud.
• Providers must use the correct cod es that correspond t o the type
of service provided
• Provider should not bill for missed appointments.
• Providers must only bill for the dates when services were actually
performed.
VACCINE ADMINISTRATION REPORTING CHANGES-
INCLU D IN G THE V F C PROG RAM
The Affordable Care Act (ACA) mandates that vaccine administration fees paid to certain
physicians and other providers administering vaccines to Medicaid-enrolled members, including
those administered to children under the Vaccines for Children program, be increased as of
January 1, 2013. AHCCCS is currently revising our systems to allow physicians who qualify for
the increased administration fee to receive those fees for vaccine administrations. The
methodology and payment of the enhanced rate requires CMS approval, which could be delayed
as late as July 1, 2013. Therefore enhanced payments for qualifying claims with dates of service
on or after January 1, 2013 will not begin January 1 but will be made retroactively once CMS
approval is received.
In addition to the increased fees for vaccine administrations, final regulations implementing this
section of the ACA requires that vaccines be reported in a different manner than AHCCCS has
utilized in the past. Previously, vaccines were reported with the CPT codes that identified the
particular vaccines given, and for VFC, the SL modifier was attached to that vaccine code.
Physicians and other providers also reported one vaccine administration code, which was not
separately paid, regardless of how many vaccines were administered on that date of service.
With the changes under the ACA, both the specific vaccine code and the vaccine administration
code must be reported by all providers reporting vaccine administration services. If the vaccine
is provided through the VFC program, the SL modifier must be added to both the vaccine code
and the vaccine administration code. Do not add the SL modifier to vaccine and

administration codes used to report services provided to members who are over 18 years of age
or for vaccines that are not covered under the VFC program administered to children.
CPT codes identifying the vaccine or toxoid given under the VFC program should be identified
with the appropriate CPT code to identify the vaccine, the SL modifier, and the charge listed as
$0.00. Vaccines should be identified with the appropriate CPT code and the charge for that
vaccine for members 18 years of age or older or for vaccines not covered under the VFC
program.
When vaccines are administered separately, i.e., through separate injections, an administration
fee will be paid for each separate administration. Additional administration fees are not paid
when multiple vaccines are administered through a single injection. Physicians should not
separate vaccine toxoids typically administered together into separate syringes to report multiple
vaccine administration codes.
Reporting multiple injections depends on which vaccine administration codes are used to report
the services. When more than one vaccine is administered with counseling to a member 18 years
of age or younger, each injection is reported with CPT code 90460 and SL modifier. Providers
will be paid a separate fee for each injection. If more than one vaccine/toxoid is included in a
single injection, the additional toxoids should be identified with the appropriate CPT code and
the administrations of those other toxoids may be identified with CPT code 90461. AHCCCS
will not make additional payment for administration of other additional toxoids included in the
injection identified with CPT code 90460 and providers are not compelled to report 90461 for
the administration of those additional toxoids.
When more than one injection is given to a member who is over the age of 18 or to a child
without counseling, the administration of the first injection is identified with CPT code 90471
and additional injections are identified with CPT code 90472. Each vaccine or toxoid
component should be identified with the appropriate CPT code on the claim form along with the
charge for that toxoid. When more than one toxoid is included in the injection, each toxoid
should be listed but only one administration code is reported (90471 for a single injection; 90471
and 90472 for multiple injections).
For example, a DTaP vaccine should continue to be administered through a single syringe and
the physician should report a single administration code even though three vaccine toxoids are
included in that syringe. If, however, the physician also administers a Hepatitis B vaccine
through a separate injection site, s/he may report a second administration code. Please refer to
the “New Requirements for Submission of Claims for Vaccine Administration” FAQs for more
information at http://www.azahcccs.gov/commercial/ProviderBilling/rates/PCSrates.aspx
New Requirements for Submission of Claims for Vaccine Administ ration
Frequently Asked Questions
Revision Date: 2/11/2013 (Vaccine code examples have been amended & additional FAQs
appended)
Q1
When does the provider need to start billing using the new methodology?
A1
Per the federal requirements, January 1, 2013.
Q2
Do all providers need to use the new claims billing method?
A2
Yes, all providers need to use the new claims billing method.
Q3
When will eligible providers see an increase from the current VFC administration
rate?
A3
Enhanced payments for qualifying claims with dates of service on or after January 1,
2013 will not begin January 1 but will be made retroactively once CMS approval of the
required Arizona state plan amendment and methodology is received. Providers must
meet the requirements as noted in the 12/11/12 memo
http://www.azahcccs.gov/commercial/downloads/rates/PCPInfoMemo.pdf
to be eligible for the enhanced payment. CMS approval may delayed as late as July 1,
2013.
Q4
Is the SL modifier used for both the vaccine and the vaccine administration codes?
A4
Yes, the SL modifier is used for both the vaccine and the vaccine administration codes
under VFC only. Vaccines for adults or non-VFC vaccines for children do not have the
SL modifier added.
Q5
Will providers only receive payment for one administration code regardless of how
many vaccines were administered?
A5
No, if the provider individually administers more than one vaccine, the provider can bill
for the administration of each vaccine, provided the additional vaccines are
administered through a separate injection. The provider will not be paid for additional
toxoids in the same syringe. This mirrors the current payment policy.
Providers cannot divide vaccines commonly administered in a single injection in order
to report multiple administrations. When medically necessary and appropriate to
administer a second injection, a second administration fee may be paid.
Q6
Is 90461 an open code?
A6
AHCCCS has opened this add-on code as of 1/1/13. However, under VFC no additional
payment is made for additional toxoids in the same syringe.
Q7
Can AHCCCS provide examples of code use?
A7
The following examples illustrate several vaccine coding situations
With the changes under the ACA, both the specific vaccine code and the vaccine
administration code must be reported by all providers reporting vaccine administration
services.
• If the vaccine is provided through the VFC program, the SL modifier must be
added to both the vaccine code and the vaccine administration code. Do not
add the SL modifier to vaccine and administration codes used to report services
provided to members who are over 18 years of age or for vaccines not covered
under the VFC program administered to children.
• CPT codes identifying the vaccine or toxoid given under the VFC program
should be identified with the appropriate CPT code to identify the vaccine, the
SL modifier, and the charge listed as $0.00.
• Vaccines for members 18 years of age or older or for vaccines not covered
under the VFC program should be identified with the appropriate CPT code and
the charge for that vaccine.
As noted in Q5, more than one vaccine administration payment can be made if multiple
injections are given to the member. Reporting multiple injections depends on which
vaccine administration codes are used to report the services. When more than one
vaccine is administered with counseling to a member 18 years of age or younger, each
injection is reported with CPT code 90460. Providers will be paid a separate fee for
each injection. If more than one vaccine/toxoid is included in a single injection, the
additional toxoids should be identified with the appropriate CPT code and the
administrations of those other toxoids may be identified with CPT code 90461.
AHCCCS will not make additional payment for administration of other additional
toxoids included in the injection identified with CPT code 90460. Providers are not
compelled to report 90461 for the administration of those additional toxoids.
When more than one injection is given to a member who is over the age of 18 or to a
child without counseling, the administration of the first injection is identified with CPT
code 90471 and additional injections are identified with CPT code 90472. Each vaccine
or toxoid component should be identified with the appropriate CPT code on the claim
form along with the charge for that toxoid. When more than one toxoid is included in
the injection, each toxoid should be listed but only one administration code is reported
(90471 for a single injection; 90471 and 90472 for multiple injections).
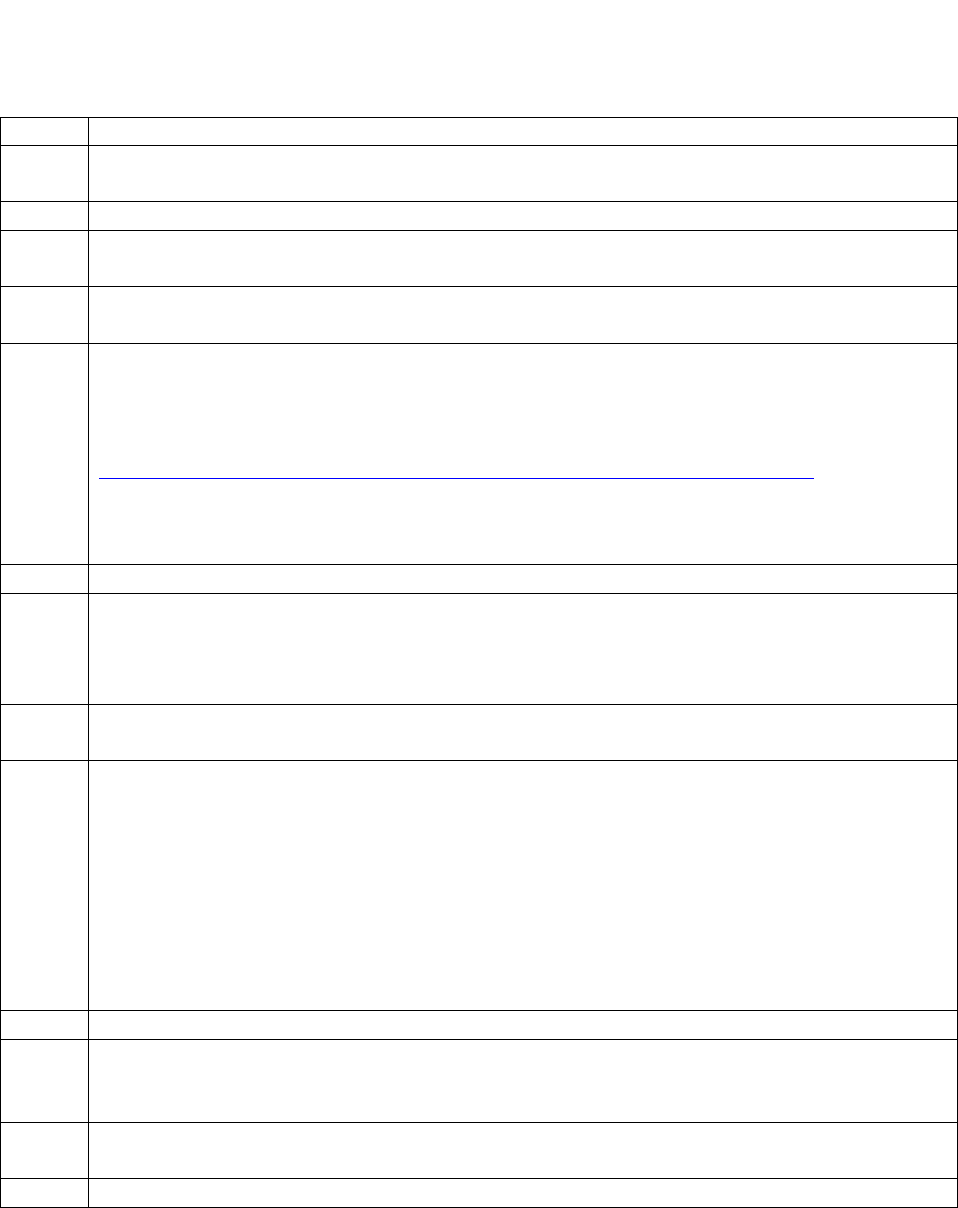
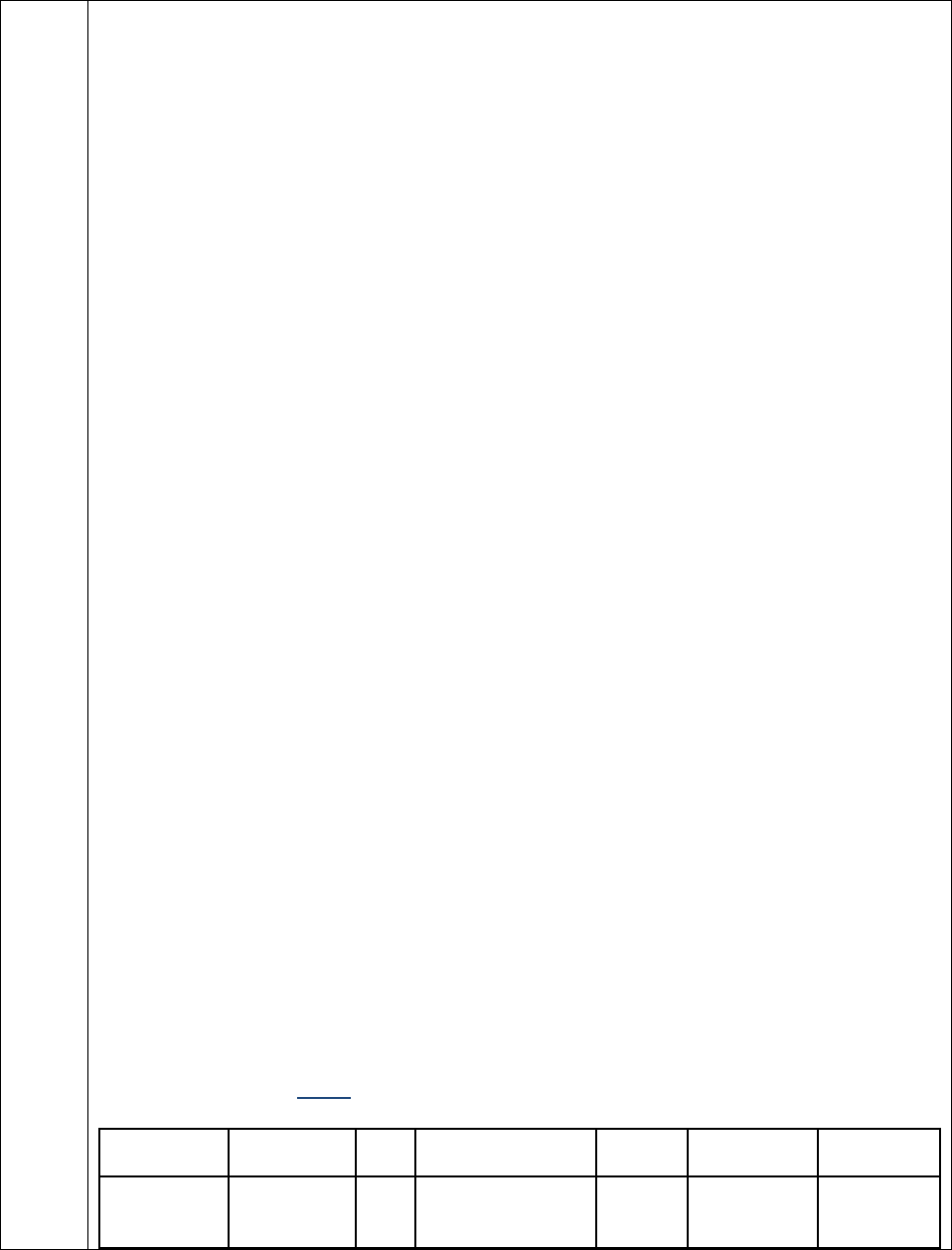
Example 1 child 18 or under receiving one injection
24. A
B
C
D
E
F
G
Dates of
Service
Place of
Service
EMG
Procedures, Services
or Supplies
Diagnosis
Pointer
$ Charges
Units
1/1/13-1/1/13
11
90460 SL
1
$xx.xx
1
1/1/13-1/1/13
11
90700 SL
1
0.00
1
Example 2 child 18 or under receiving three separate injections
24. A
B
C
D
E
F
G
Dates of
Service
Place of
Service
EMG
Procedures, Services
or Supplies
Diagnosis
Pointer
$ Charges
Units
1/1/13-1/1/13
11
90460 SL
1
$xx.xx
3
1/1/13-1/1/13
11
90700 SL
1
0.00
1
1/1/13-1/1/13
11
90655 SL
1
0.00
1
1/1/13-1/1/13
11
90707 SL
1
0.00
1
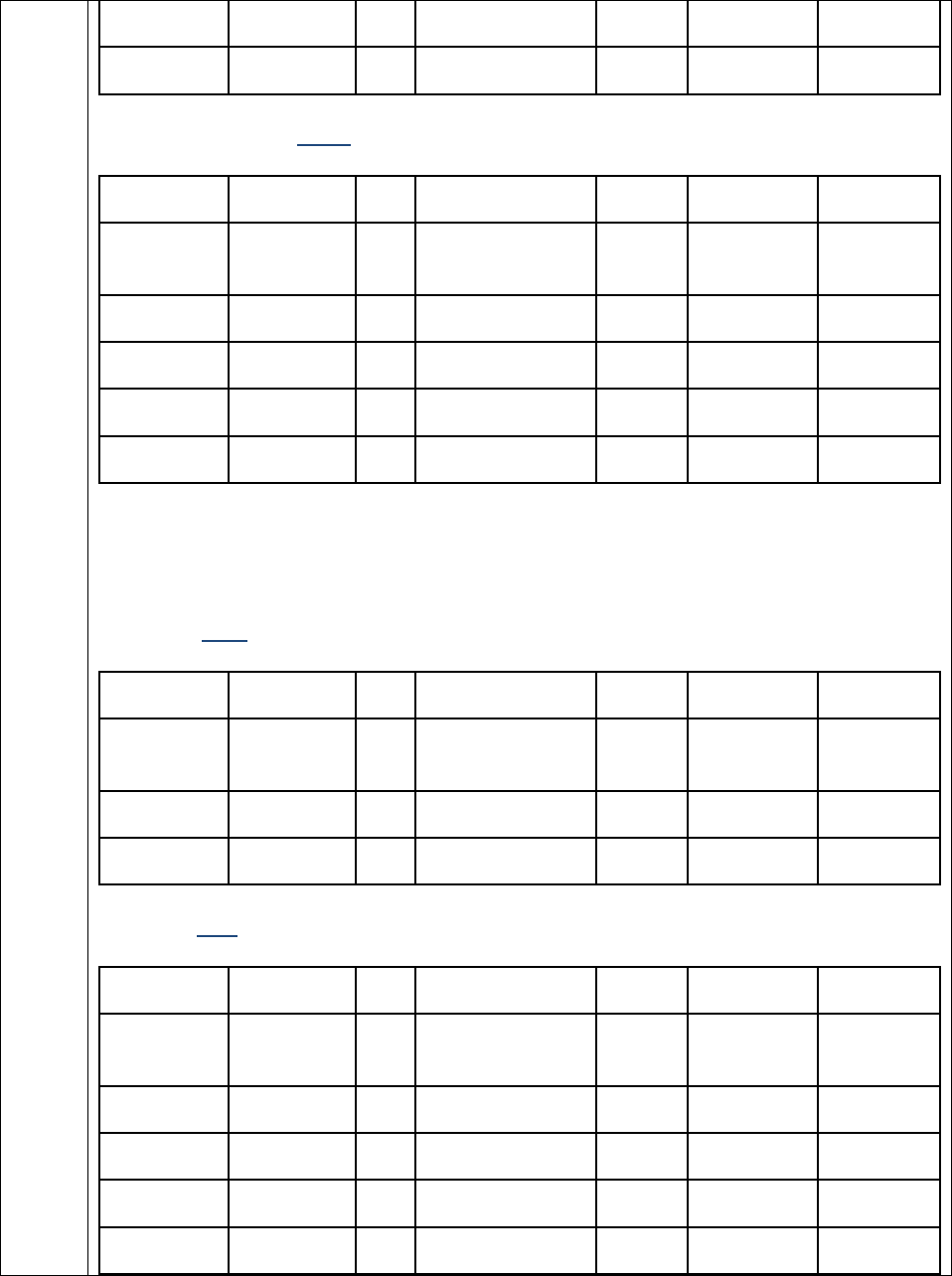
Example 3 over 18 receiving one injection
24. A
B
C
D
E
F
G
Dates of
Service
Place of
Service
EMG
Procedures, Services
or Supplies
Diagnosis
Pointer
$ Charges
Units
1/1/13-1/1/13
11
90471
1
$xx.xx
1
1/1/13-1/1/13
11
90656
1
$xx.xx
1
Example 4 over 18 receiving three injections
24. A
B
C
D
E
F
G
Dates of
Service
Place of
Service
EMG
Procedures, Services
or Supplies
Diagnosis
Pointer
$ Charges
Units
1/1/13-1/1/13
11
90471
1
$xx.xx
1
1/1/13-1/1/13
11
90472
1
$xx.xx
2
1/1/13-1/1/13
11
90656
1
$xx.xx
1
1/1/13-1/1/13
11
90670
1
$xx.xx
1
1/1/13-1/1/13
11
90703
1
$xx.xx
1
Q8
Are G0008, G0009 and G0010 administration codes eligible for the enhanced rate?
A8
No they are not. Under 42 CFR 447.400, only CPT codes 90460, 90461, 90471, 90472,
90473 and 90474 or their successor codes are eligible for the enhanced rate. Note that these
codes are eligible for the enhanced rate only if they are open codes within the State
Medicaid program.
Q9
Recently several specialty societies issued guidance directing providers reporting
vaccine and vaccine administration services on the same date of service as an
Evaluation and Management (E&M) service, including Preventive Med i cin e
exams, to add Modifier 25 to the E&M code. Do these instructions apply to claims
submitted to AHCCCS?
A9
CMS has added numerous code pairs to the Correct Coding Initiative (CCI) list of codes
Procedure to Procedure code edits. These new edits, effective 1/1/13, pair the vaccine
administration codes (90460, 90461, and 90471-90474) with the E&M codes. These
CCI edits do not allow both the vaccine administration service and the E&M service to
be paid for the same date of service unless the E&M service is identified with modifier
25. AHCCCS must adopt these CCI edits. Providers administering vaccines and
performing an E&M service on the same date of service must add modifier 25 to the
E&M code. Modifier 25 is not added to the vaccine administration codes.
Q10
Will the AHCCCS VFC administration rate increase to the new regional
maximum for all providers?
A10
No. AHCCCS has elected not to adopt the new regional maximum VFC
rate. Providers who are eligible for enhanced payment rates will receive the enhanced
rate of $21.33 for vaccine administration under VFC.
For all other vaccine administrations under VFC, the AHCCCS rate of $15.43 remains
unchanged.
GENERAL REMINDERS FROM THE UM/CM UNIT’S PA UNIT
Lodging Providers (provide r t ypes 55 & 56):
Effec t ive 01/01/2013, lodging services will require prio r authorization. Providers can
fax l odging requests to the UM/CM Unit’s FFS Prior Authorization area, wit h
supporting documentation, us ing the completed Fee For Servi ce Authorization
Request form. Use of the FFS Author ization Request Form is mandatory. Some of the
information that should be provided with your lodging request is:

What care member is receiv in g
Why mem ber needs lodging
Information supporting the numb er of nights requested for lodg ing
Dates and times of all appointments and/or p rocedures occurring during the lodging
dates
MD name
Facilit y name
Escort name an d relatio n ship, when app licable
HCPCS codes for lodging services
Dollar amount requested for each HCP CS code Invoice
Transportation Reminders:
Some NEMT providers are not using the FFS mandatory forms when submitting
transport documentat ion. These forms must be present when faxing infor mation to
the FFS Prior Authorization area or your documents will b e returned.
Reminder: Extra miles billed becau se a provider is dropping off members at the home
of a family ’s member will be denied. This is not a covered transport ation service.
The preferred method of requesting an authorization fo r transportation services is via
the online system. Please keep in mind that NEMT services and Lodging services are
two separate services and should not be confused with one another.
When submitting a request to correct a p reviously authorized date of service, please
fax a request to revoke the old date of service usin g the FFS Authorization Correction
form af ter entering your n ew authorization request for t he new date of service
online. Corrections to d ate of service are st ill subject to guidelines related to
timeliness. Authorization requests and corrections to date of service should occur
before the s ervice is rendered.
Once a member’s eligibility posts to the system, NEMT authoriz ation requests for the
date the eligibility posted and forward are subject to guidelines regarding timeliness



