Fillable Printable Form 417
Fillable Printable Form 417
Form 417

AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 400 - OPERATIONS
417- Page 1 of 6
417 - APPOINTMENT AVAILABILITY, MONITORING AND REPORTING
EFFECTIVE DATES: 10/01/12, 10/01/13, 04/01/15, 07/01/16, 10/01/16, 10/01/17
REVISION DATES: 01/08/08, 06/26/12, 10/24/12, 07/03/13, 03/05/15, 04/02/15, 05/11/16,
10/20/16, 03/30/17, 06/15/17
I. PURPOSE
This Policy applies to Acute Care, ALTCS/EPD, CRS, DCS/CMDP (CMDP), DES/DDD
(DDD), and RBHA Contractors. The policy establishes appointment accessibility and
availability standards to ensure Contractor compliance with AHCCCS network sufficiency
requirements. The standards delineated in this policy establish a common process for
Contractors to monitor and report appointment accessibility and availability. These policy
requirements do not apply to emergency conditions
II. DEFINITIONS
1800 REPORT
ESTABLISHED
PATIENT
NEW PATIENT
URGENT CARE
APPOINTMENT
An AHCCCS generated document, provided quarterly, that
identifies Primary Care Physicians (PCPs) with a panel of more
than 1800 AHCCCS members.
A member who has received professional services from the
physician or any other physician with that specific subspecialty
that belongs to the same group practice, within the past three
years from the date of appointment.
A member who has not received any professional services from
the physician or another physician with that specific specialty
and subspecialty that belongs to the same group practice, within
the past three years from the date of appointment.
An appointment for medically necessary services to prevent
deterioration of health following the acute onset of an illness,
injury, condition, or exacerbation of symptoms.
III. POLICY
A. MONITORING APPOINTMENT STANDARDS
1. The Contractor is responsible for providing services that are sufficient in amount,
duration and scope to reasonably be expected to achieve the purpose for which the
services are furnished. To ensure this, the Contractor must provide a comprehensive
provider network that provides access to all services covered under the contract for all
members. If the Contractor’s network is unable to provide medically necessary
services required under contract, the Contractor must adequately and timely cover

AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 400 - OPERATIONS
417- Page 2 of 6
these services through an out of network provider until a network provider is
contracted.
2. The Contractor must ensure adherence to service accessibility standards and the
following contractual appointment standards [42 CFR 438.206].
3. The Contractor must use the results of appointment standards monitoring to assure
adequate appointment availability in order to reduce unnecessary emergency
department utilization.
4. The Contractor shall have written policies and procedures about educating its provider
network regarding appointment time requirements. The Contractor must develop a
corrective action plan when appointment standards are not met. In addition, the
Contractor must develop a corrective action plan in conjunction with the provider
when appropriate [42 CFR 438.206(c)(1)(iv), (v) and (vi)].
B. GENERAL APPOINTMENT STANDARDS FOR ALL CONTRACTORS
1. For Primary Care Provider Appointments:
a. Urgent care appointments as expeditiously as the member’s health condition
requires but no later than two business
days of request, and
b. Routine care appointments within 21 calendar days of request.
2. For Specialty Provider Referrals:
a. Urgent care appointments as expeditiously as the member’s health condition
requires but no later than three business
days from the request, and
b. Routine care appointments within 45 calendar days of referral.
3. For Dental Provider Appointments:
a. Urgent appointments as expeditiously as the member’s health condition requires
but no later than three business
days of request, and
b. Routine care appointments within 45 calendar days of request.
4. For Maternity Care Provider Appointments,
Initial prenatal care appointments for enrolled pregnant members shall be provided as
follows:
a. First trimester - within 14 calendar
days of request,
b. Second trimester within seven calendar days of request,
c. Third trimester within three days business of request, and
d. High risk pregnancies as expeditiously as the member’s health condition requires
and no later than three business days of identification of high risk by the
Contractor or maternity care provider, or immediately if an emergency exists.
AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 400 - OPERATIONS
417- Page 3 of 6
C. GENERAL BEHAVIORAL HEALTH APPOINTMENT STANDARDS FOR ACUTE,
ALTCS/EPD, CRS AND RBHA CONTRACTORS
1. For Behavioral Health Provider Appointments:
a. Urgent need appointments as expeditiously as the member’s health condition
requires but no later than 24 hours from identification of need
b. Routine care appointments:
i. Initial assessment within seven calendar days of referral or request for service,
ii. The first behavioral health service following the initial assessment as
expeditiously as the member’s health condition requires but no later than 23
calendar days after the initial assessment, and
iii. All subsequent behavioral health services, as expeditiously as the member’s
health condition requires but no later than 45 calendar
days from identification
of need.
2. For Psychotropic Medications:
a. Assess the urgency of the need immediately, and
b. Provide an appointment, if clinically indicated, with a Behavioral Health Medical
Professional within a timeframe that ensures the member a) does not run out of
needed medications, or b) does not decline in his/her behavioral health condition
prior to starting medication, but no later than 30 calendar days from the
identification of need.
D.
ADDITIONAL BEHAVIORAL HEALTH APPOINTMENT STANDARDS FOR
CRS AND RBHA
CONTRACTORS
1. For Behavioral Health Appointments for persons in legal custody of the Department
of Child Safety (DCS) and adopted children in accordance with A.R.S. §8-512.01:
a. Rapid Response when a child enters out-of-home placement within the timeframe
indicated by the behavioral health condition, but no later than 72 hours after
notification by DCS that a child has been or will be removed from their home,
b. Initial Assessment
within seven calendar days after referral or request for
behavioral health services,
c. Initial Appointment within timeframes indicated, by clinical need, but no later than
21 calendar days after the initial evaluation, and
d. Subsequent Behavioral Health Services within the timeframes according to the
needs of the person, but no longer than 21 calendar days from the identification of
need
The appointment standards for members in the legal custody of the Department of Child
Safety and adopted children are intended to monitor appointment accessibility and
availability. For additional information on behavioral health services for persons in the
legal custody of DCS and adopted children in accordance with A.R.S. §8-512.01, see
ACOM Policy 449.

AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 400 - OPERATIONS
417- Page 4 of 6
E. PROVIDER APPOINTMENT AVAILABILITY REVIEW
The Contractor is required on a quarterly basis to conduct provider appointment availability
reviews to assess the availability of Routine and Urgent appointments for Primary Care,
Specialist, Dental, CRS providers, Behavioral Health providers and Behavioral Health
appointments for persons in the legal custody of DCS. The Contractor must also review
these standards for Maternity Care providers relating to the first, second, and third
trimesters, as well as high risk pregnancies.
The Contractor must conduct provider appointment availability reviews in sufficient
quantity to ensure results are meaningful and representative of the services provided by the
Contractor’s network. Appropriate methods include:
1. Appointment schedule review where the Contractor independently validates appointment
availability,
2. Secret shopper phone calls, where the Contractor anonymously validates appointment
availability, and
3. Other methods approved by AHCCCS.
The Contractor may supplement these efforts by targeting specific providers identified
through performance monitoring systems such as the 1800 report, quality of care concerns,
complaints, grievances and the credentialing process.
To obtain approval for any additional methods, the Contractor should submit a request for
approval outlining details (including scope, selection criteria, and any tools used to collect
the information) prior to implementing the proposed method, as specified in Contract,
Section F, Attachment F3, Contractor Chart of Deliverables and RBHA Contract, Exhibit-9,
Deliverables.
F. TRACKING AND REPORTING
The Contractor must track provider compliance with appointment availability on a quarterly
basis for both New and Established Patients by Provider Type and appointment type
utilizing the reporting template, Attachment A. The Contractor must submit this
information quarterly as identified in Contract, Section F, Attachment F3, Contractor Chart
of Deliverables and RBHA Contract, Exhibit-9, Deliverables. A cover letter must be
included which summarizes the data, describes how the survey methodology is
representative of appointment standards across the Contractor’s network, explains
significant trending in either direction (positive or negative), and describes any interventions
applied to areas of concern including, any corrective actions.
In addition, annually the Contractor must summarize the results, trends, and interventions as
a component of the Network Development and Management Plan. See ACOM Policy 415
AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 400 - OPERATIONS
417- Page 5 of 6
for additional guidelines for the submission of the Network Development and Management
Plan.
The Contractor’s submission of the Network Development and Management Plan must also
include an attestation affirming the validity of the methodologies utilized and significance
of the results, along with any planned changes to the methodologies for the coming year.
AHCCCS may review Contractor monitoring and any corrective actions implemented as a
result of provider non-compliance with appointment standards.
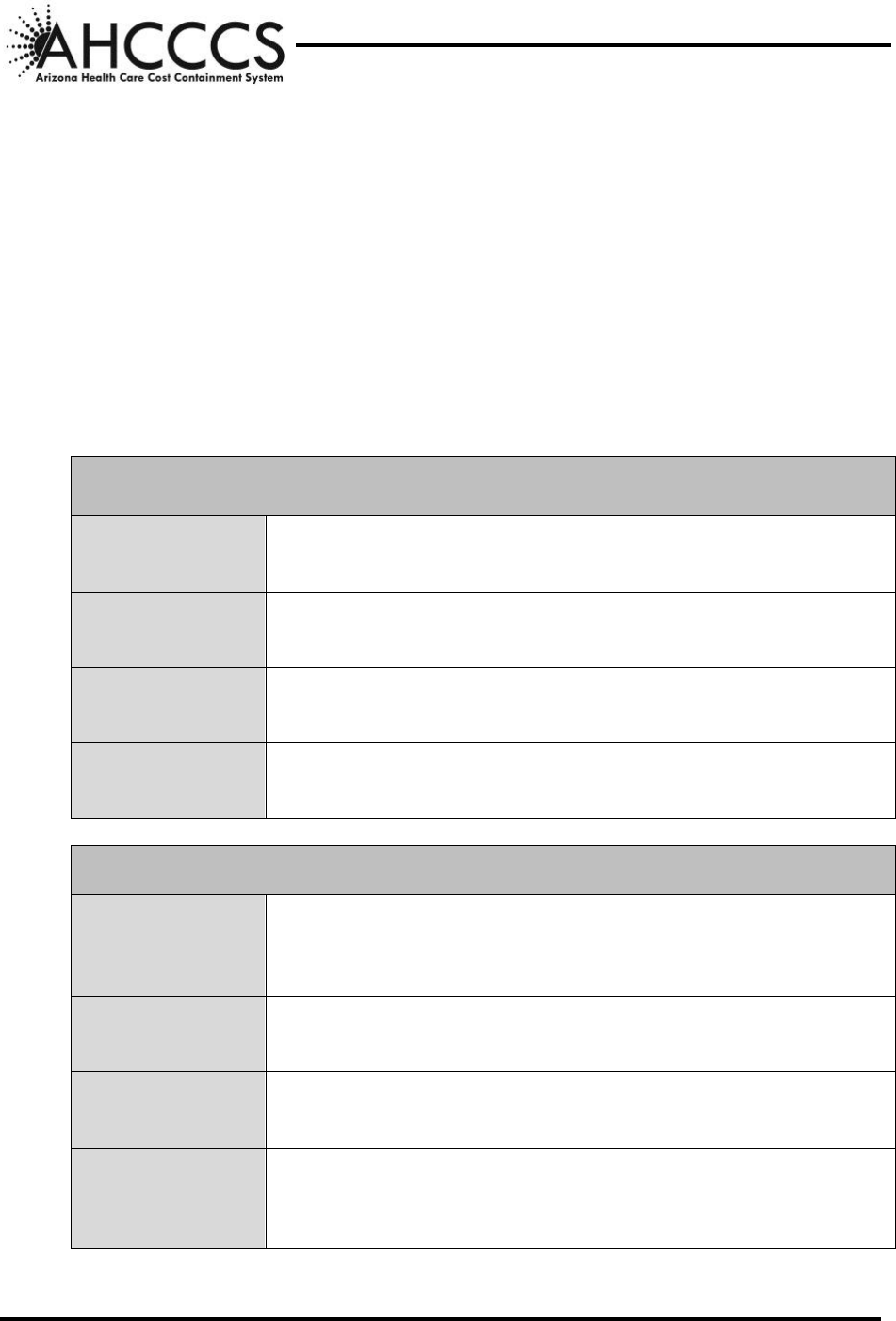
G. ATTACHMENT A, APPOINTMENT AVAILABILITY PROVIDER REPORT
Instructions for Completing Attachment A, Appointment Availability Provider Report:
PCP, SPECIALIST, AND DENTAL APPOINTMENTS
SURVEYS
Enter the number of provider surveys conducted both New and
Established patients for each provider type.
PASS
Enter the total number of providers that were in compliance with
the AHCCCS appointment standards (Urgent and Routine).
FAIL
Enter the total number of providers that were not in compliance
with the AHCCCS appointment standards.
COMPLIANCE
PERCENTAGE
The percentage of providers that are compliant with the AHCCCS
appointment standards. This field is automatically populated.
MATERNITY CARE PROVIDER APPOINTMENTS
SURVEYS
Enter the number of provider surveys conducted with Maternity
care providers related to compliance with the AHCCCS standards
for initial prenatal care appointments by trimester and risk.
PASS
Enter the total number of providers that were in compliance with
the AHCCCS appointment standards for maternity care.
FAIL
Enter the total number of providers that were not in compliance
with the AHCCCS appointment standards for maternity care.
COMPLIANCE
PERCENTAGE
The percentage of providers that are compliant with the AHCCCS
appointment standards for maternity care. This field is
automatically populated.
AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 400 - OPERATIONS
417- Page 6 of 6
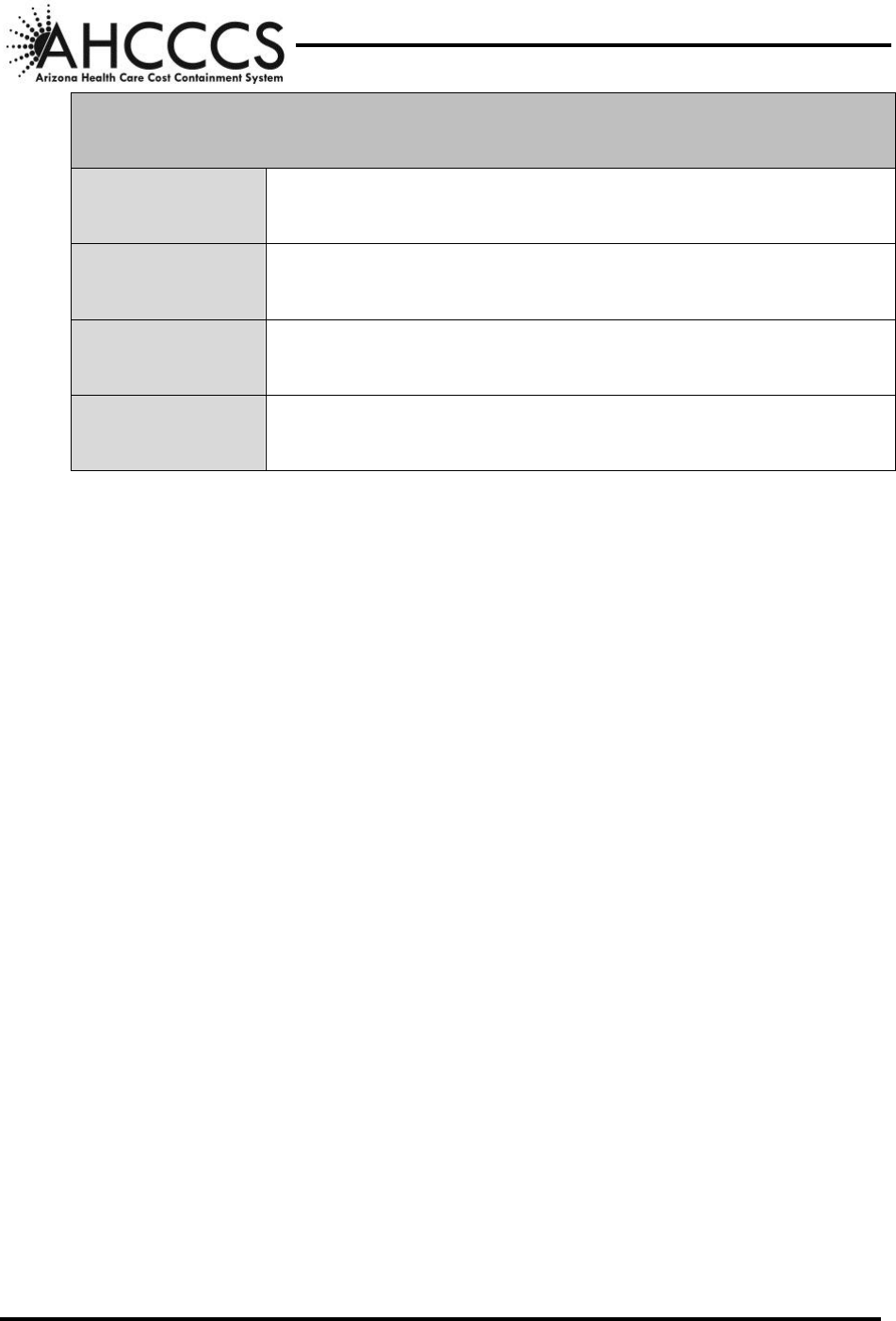
BEHAVIORAL HEALTH, AND REPORT FOR PERSONS IN DCS CUSTODY
APPOINTMENTS
SURVEYS
Enter the number of provider surveys conducted for each
behavioral health appointment category.
PASS
Enter the total number of providers that were in compliance with
the AHCCCS appointment standards.
FAIL
Enter the total number of providers that were not in compliance
with the AHCCCS appointment standards.
COMPLIANCE
PERCENTAGE
The percentage of providers that are compliant with the AHCCCS
appointment standards. This field is automatically populated.



