Fillable Printable Form 5217
Fillable Printable Form 5217
Form 5217
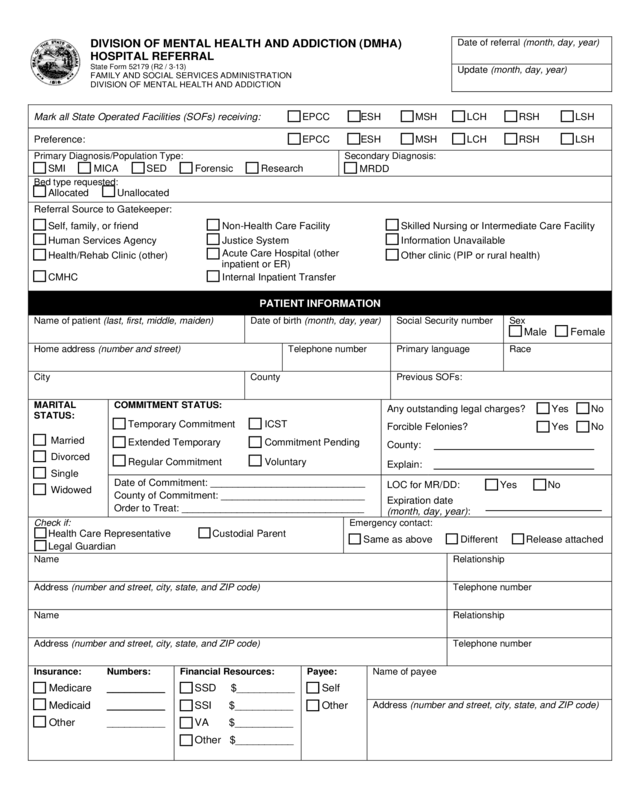
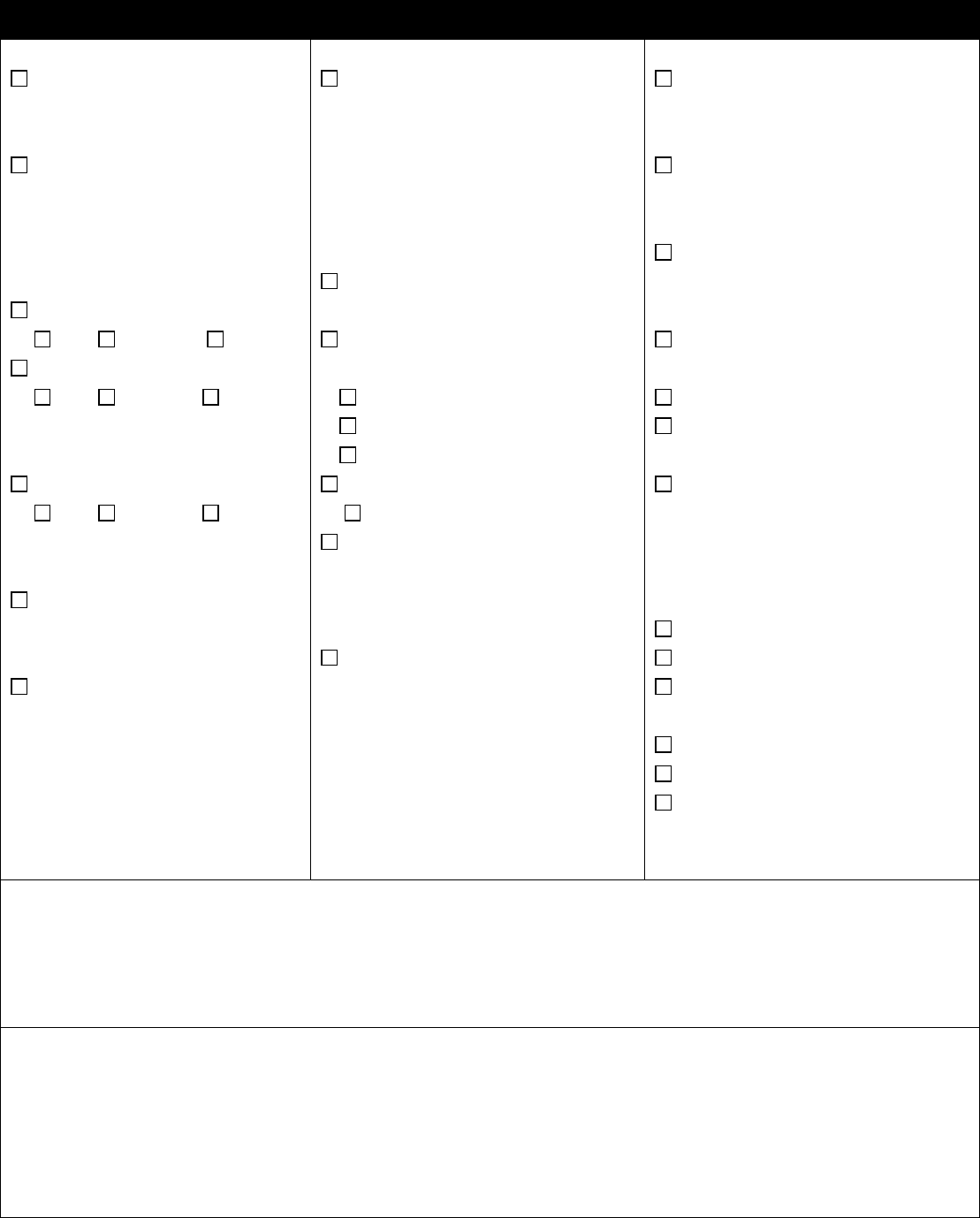
DIVISION OF MENTAL HEALTH AND ADDICTION (DMHA)
HOSPITAL REFERRAL
State Form 52179 (R2 / 3-13)
FAMILY AND SOCIAL SERVICES ADMINISTRATION
DIVISION OF MENTAL HEALTH AND ADDICTION
Date of referral (month, day, year)
Update (month, day, year)
Mark all State Operated Facilities (SOFs) receiving: EPCC ESH MSH LCH RSH LSH
Preference: EPCC ESH MSH LCH RSH LSH
Primary Diagnosis/Population Type:
SMI MICA SED Forensic Research
Secondary Dia gnosis:
MRDD
Bed type requested:
Allocated Unallocated
Referral Source to Gatekeeper:
Self, family, or friend Non-Health Care Facility Skilled Nursing or Intermediate Care Facility
Human Services Agency Justice System Information Unavailable
Health/Rehab Clinic (other)
Acute Care Hospital (other
inpatient or ER)
Other clinic (PIP or rural health)
CMHC Internal Inpatient Transfer
PATIENT INFORMATION
Name of patient (last, first, middle, maiden)
Date of birth (month, day, year)
Social Security number
Sex
Male Female
Home address (number and street)
Telephone number
Primary language
Race
City
County
Previous SOFs:
MARITAL
STATUS:
Married
Divorced
Single
Widowed
COMMITMENT STATUS:
Any outstanding legal charges? Yes No
Temporary Commitment ICST
Forcible Felonies?
Yes No
Extended Temporary Commitment Pending
County: _____________________________
Regular Commitment Voluntary
Explain: _____________________________
Date of Commitment: ____________________________
County of Commitment: __________________________
Order to Treat: _________________________________
LOC for MR/DD:
Yes No
Expiration date
(month, day, year):
_____________________
Check if:
Health Care Representative Custodial Parent
Legal Guardian
Emergency contact:
Same as above Different Release attached
Name
Relationship
Address (number and street, city, state, and ZIP code)
Telephone number
Name
Relationship
Address (number and street, city, state, and ZIP code)
Telephone number
Insurance:
Medicare
Medicaid
Other
Numbers:
__________
__________
__________
Financial Resources:
SSD $__________
SSI $__________
VA $__________
Other $__________
Payee:
Self
Other
Name of payee
Address (number and street, city, state, and ZIP code)
Reset Form
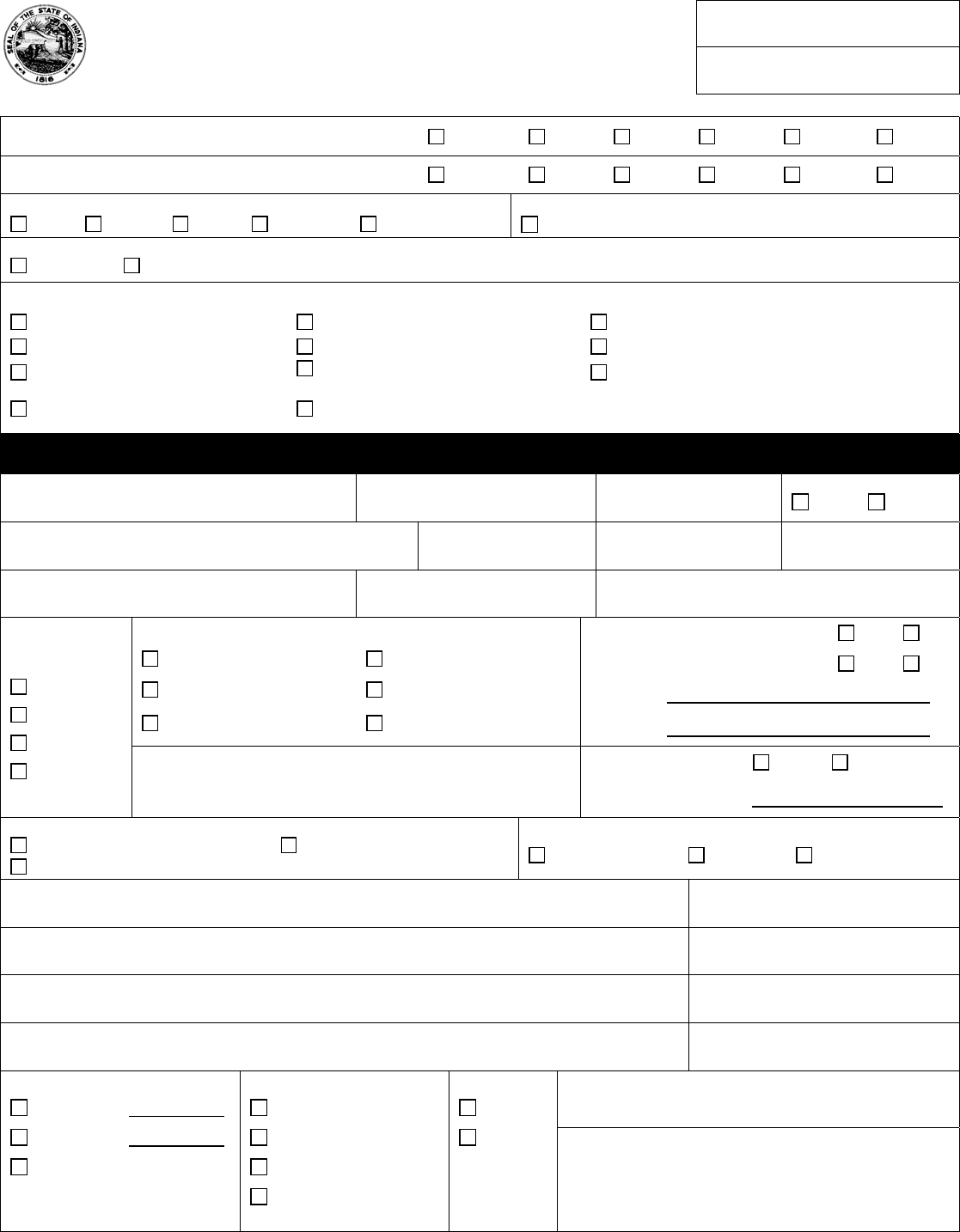
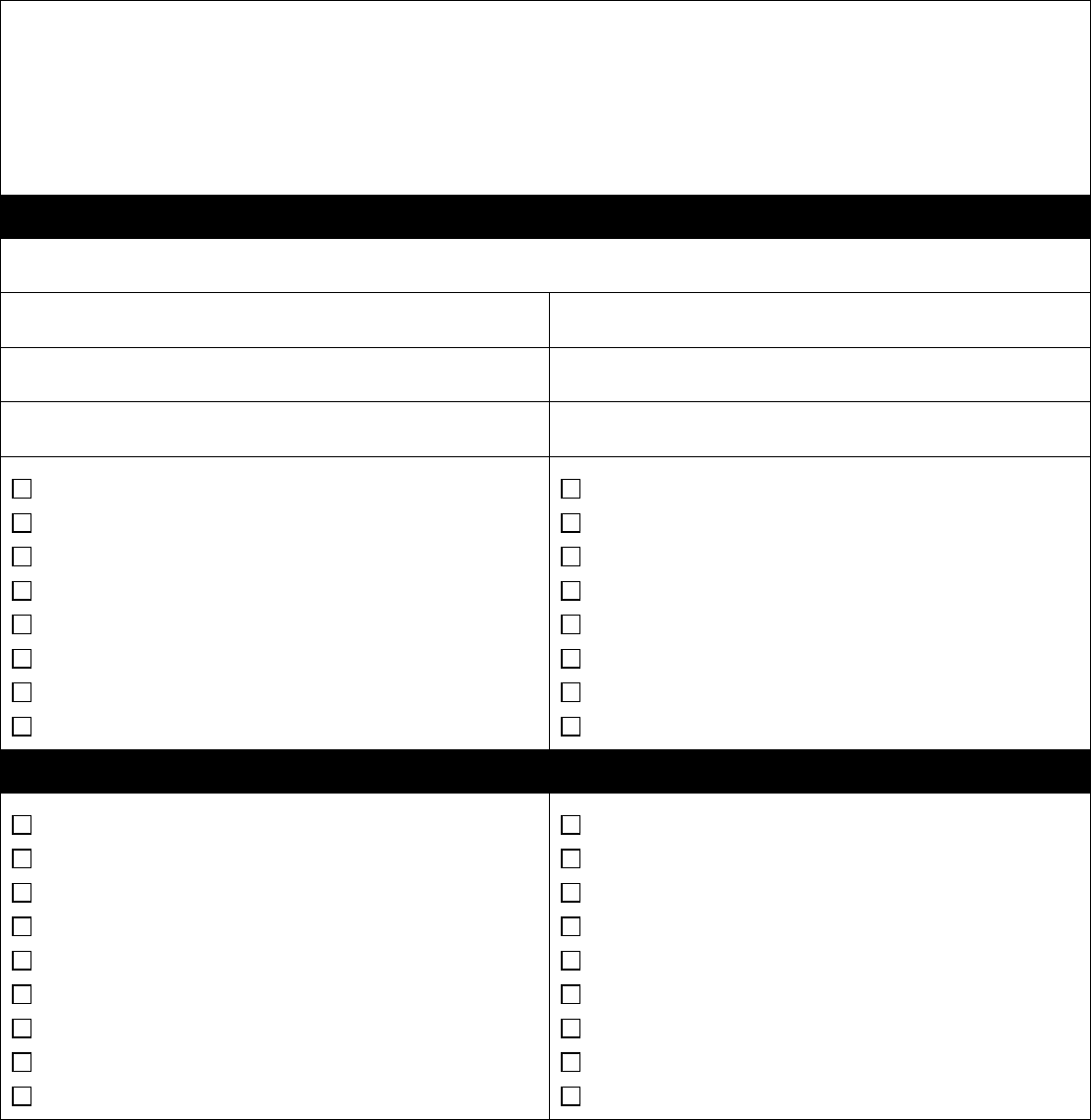
PSYCHIATRIC INFORMATION
Current placement
Date admitted (month, day, year)
Address (number and street, city, state, and ZIP code)
Diagnosis Axis I
Axis II
Axis III
GAF: Past 12 months
GAF: Current
IQ (MR/DD):
Current Symptoms and Behaviors :
Reason for Hospitalization
RECOVERY NEED
Select 2:
1 = Primary Treatment Need
2 = Secondary Treatment Need
COMMUNITY INTEGRATION
TRAINING MODULES
Defined From “Recovery Need”
Select 2
SPECIALIZED
TREATMENT PROGRAMMING
Defined From “Recovery Need”
Select 1 (1 from Each Subcategory)
Stabilization of Psychiatric Symptoms
Socialization Skills
Coping Skills
Stress Identification
Problem Solving Skills
Communication Skills
Health Education & Awareness
Nutritional Education
Money Management
Vocational Preparation
Resource Linkage
Support System Development
Other: ______________________________
MI + Addiction Treatment
Sexual Responsibility Training
Borderline Treatment Program
Polydipsia &/or Fluid Management
MI + MRDD
Eating Disorder
PTSD – Combat Related
Impairment (Select 1)
Physical Disability
Visual
Deaf
Mobility
______________________
Adaptive Equipment Needs
Overt Aggression (Select 1)
Verbal
Physical - Objects
Physical - Self
Physical - Others
Other: _________________________
Reduction of Aggressive Behavior
Improved Medication Management
Improved Treatment Plan Participation
Community Integration Training
Specialized Treatment Programming
Completion of Substance Abuse Program
Reduction of Inappropriate Sexual Behaviors
School or Educational Programming
Increased Diagnosis Awareness
Demonstration of Behavior Mod Skills
Increased ADL Proficiency
Stabilization of Medical or Nursing Issues
Reduction of Self Harming Behavior
Legal Education
Restoration of Competency
Other: ________________________________
Specify measur able recovery goals related to the treatment needs noted above:
Goal for primary treatment need:
Goal for secondary treatment need:
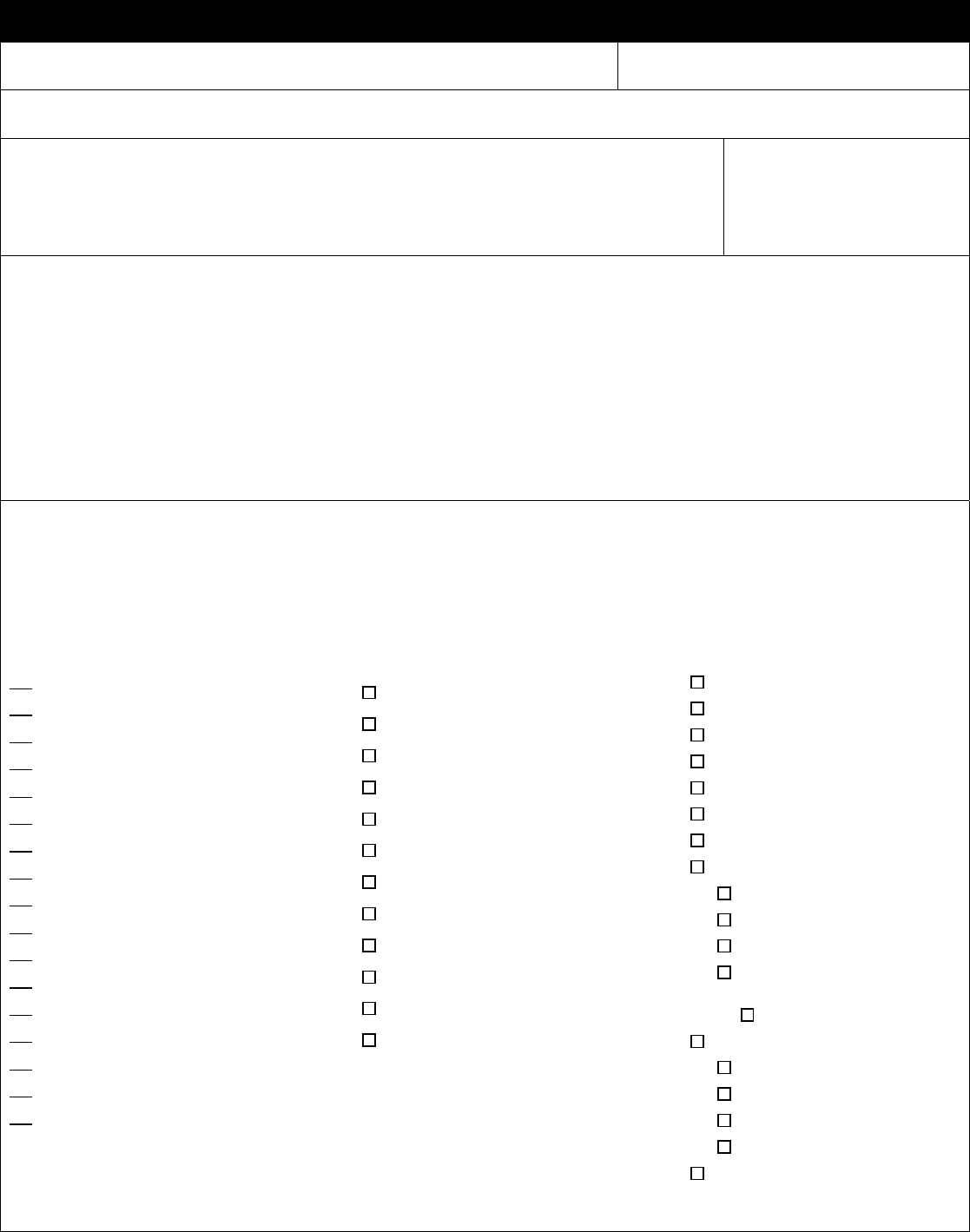
ANTICIPATED LENGTH OF STAY AND PLA CEM ENT AVAILA BILITY UPON DISCHARGE
Exists
Development
Required
Full with Wait List
Exists Out of Home
Area
Does not Exist
without
Modification
1 - 6 months 6 7 8 9 10
6 – 12 months 11 12 13 14 15
1 – 2 years 16 17 18 19 20
2 – 3 years 21 22 23 24 25
Has the Patient Experienced or Demonstrated (Check all that apply):
Violence to self within last six (6) months
Last date (month, day, year): ________________________________________
Specify: _________________________________________________________________________________________ ___
Violence to others within last six (6) months
Last date (month, day, year): ________________________________________
Specify: _________________________________________________________________________________________ ___
Substance abuse within last six (6) months
Last date (month, day, year): ________________________________________
Substance type: ___________________________________________________________________________________ __
Psychological Trauma (at any time – includes physical, sexual, emotional abuse and/or severe childhood neglect):
Substance type: ___________________________________________________________________________________ __
History or Current Suicidal Ideation
Current Medications and Dosages:
Medications Recently Changed and Reason:
TREATING PHYSICIAN
Name of physician
Telephone number
MEDICAL NEEDS / SPECIAL NEEDS
Diet
Specify: __________________
_________________________
Mobility
Restrictions:_______________
_________________________
Assistive Devices:__________
_________________________
Fall Risk
Low Moderate High
Hearing Impairment
Mild Moderate Severe
Assistive Devices:__________
_________________________
Visual Impairment
Mild Moderate Severe
Assistive Devices:__________
_________________________
Other Medical Equipment
Specify: __________________
_________________________
Communication Difficulty
Assistive Devices:__________
_________________________
Past History of T.B.
Current PPD:
Results: _________________
Date: __________
Chest X-Ray:
Results: _______________
Date: _________________
Communicable Disease
Specify: __________________
Communicable &/or Infectious
Disease History
History of MRSA
History of Multi-drug
Resistant Organisms.
Diabetes
Insulin Dependent
Allergies
List:_______________________
___________________________
___________________________
Surgeries Within the Last 12 Months
Specify: _____________________
____________________________
Circulatory Issues (Heart Disease,
HTN, etc.)
Specify: ______________________
Respiratory (COPD, asthma)
Specify: ______________________
Assistive Devices:______________
GI Tract (ulcers, gastric reflux,
colostomy G-tube, etc.)
Specify: ______________________
GU Tract - Urinary (dialysis,
incontinence, catheter, etc.)
Polydipsia
Integumentary System (Skin Issues)
Specify: ______________________
Neurological (seizures, NMS, altered
gait)
Specify: ______________________
Smoking History
Currently smokes: amt/day ________
Quit smoking less than 1 year ago
Never smoked
Received counseling for smoking:
Yes Approx date: __________
No
Currently uses other tobacco products
Type: ______________________
Provide additional information regarding the current treatment of items specified in Medical/Special Needs section (as
applicable).
A copy of current physical may be used if current treatment is included. Attach additional sheets if necessary.
ANSA/CANS Completion Date (month, day, year): _______________________ LON: __________________________
Patient strengths:
a) ___________________________________________________________________________________________
b) ___________________________________________________________________________________________
c) ___________________________________________________________________________________________
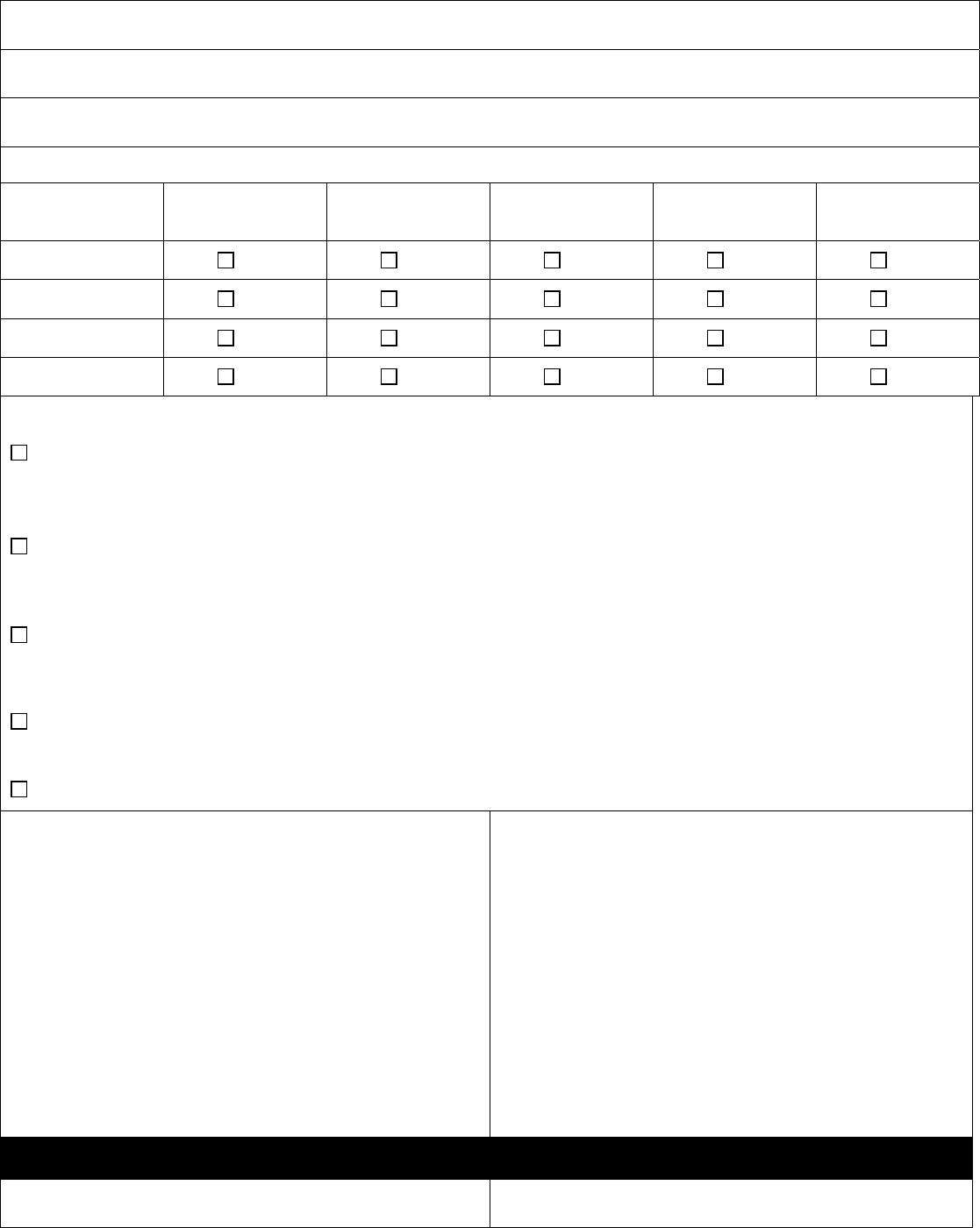
GATEKEEPER / DISCHARGE PLAN - Community Placement Needs
Name of agency
Gatekeeping Liaison Coordinating Admission/Discharge
Telephone number
Address (number and street)
Date (month, day, year)
City / State / ZIP code
Signature
SGL (24hr) SMI
SGL (24hr) MR/DD
MRDD Supported Living Waiver
MRDD ICF/MR Facility
Family Personal Home
Specialized Residential Facility
Medical or Nursing Facility
Cluster Apt. Setting or SILP
DOC (forensic only)
Subacute
MRDD ESN
Children’s Residential Facility
Halfway Program – Chemical Addiction
AFA
Therapeutic Foster Care
Other: ______________________________________
GATEKEEPER / DISCHARGE PLAN - Post SOF Community Program Needs
AIRS / CAIRS
Intensive Outpatient
Medication Evaluation & Monitoring
Case Management
Substance Abuse Aftercare
Vocational & Employment Services
ACT – Assertive Community Treatment
IDDT – Integrated Dual Diagnosis Treatment
ATR – Access to Recovery
SOC – Systems of Care (SED)
Children’s Medicaid Waiver
Behavioral Modification & Support
Community Habilitation
Health Care Coordination
Prevocational/Sheltered Employment
Supportive/Supported Housing
IMR – Illness Management and Recovery Program
Other: ______________________________________
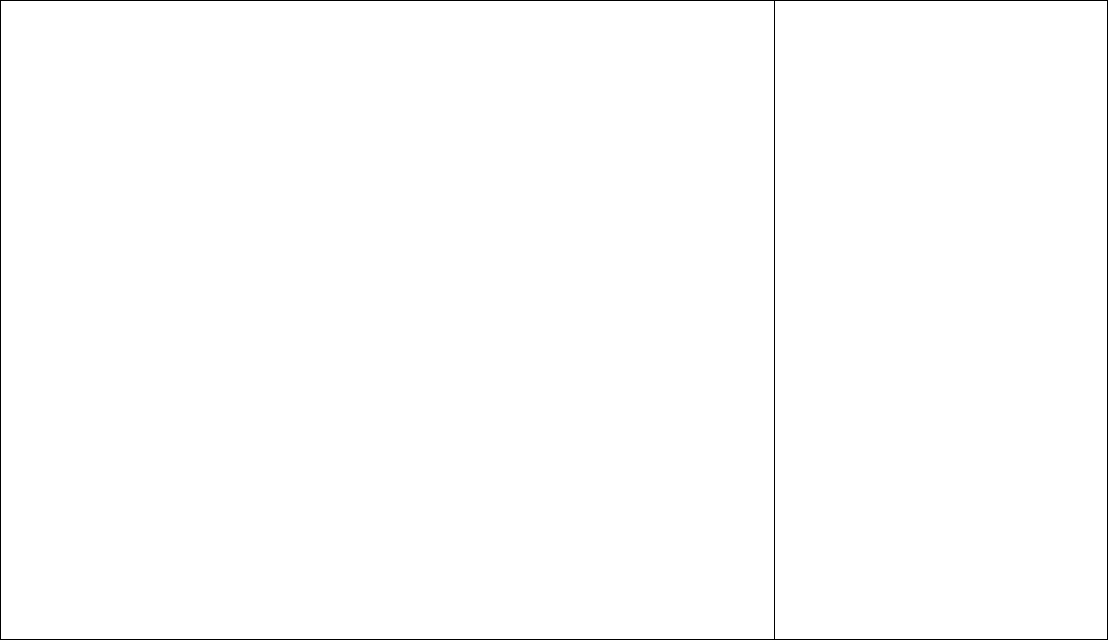
Required Signatures:
Consumer:
________________________________________________________
Consumer Signature &/or Parent or Guardi an
________________________________________________________
Witness if No Consumer Signature
Gatekeeping Staff Completing Referral on Behalf of Agency:
________________________________________________________
Staff Signature
________________________________________________________
Title / Agency &/or Unit
________________________________________________________
Telephone number
Date (month, day, year)
______________________
______________________
______________________
DMHA HOSPITAL REFERRAL FORM DIRECTIONS
When referral to a DMHA hospital is determined appropriate by the Gatekeeper, the DMHA Hospital Referral
Form is to be completed, signed by the Gatekeeper and forwarded to the appropriate hospital with the
supporting documents listed below. Upon receipt of the form and required documents, the hospital admissions
team will review and contact the Gatekeeper within five working days regarding service appropriateness, bed
availability, and waiting list.
The following documents are required with the Admission Referral Form:
Current mental status (most recent psychiatric assessment) and significant findings
Current risk factors (self-harm, aggression, elopement, falls, etc.)
Current full physical examination within 30 days of admission
Any pertinent medical workups including labs within 30 days of referral
Commitment papers (or as soon as available; must be prior to admission)
Legal papers (guardianship, wardship, Advance directives, DNR’s, 4CR designations, probation
contacts/status, status of legal charges, etc.)
Current treatment plan (include current medications with dosages)
Current psychological testing scores if available
Identification Verification (state issued picture IDs, drivers license (if applicable), birth certificate, etc.)
All available financial information (Medicaid/Medicare cards, SS cards, income verification, etc)
Result of TB test (date given and read). Test given within 30 days of referral but required within 90
days prior to admission.
ANSA/CANS (within 30 days of referral and updated every 90 days if waiting)
Additional documentation is required for referrals with secondary MR/DD diagnosis and Child/Youth referrals:
Referrals with Secondary MR/DD:
Diagnostic and Evaluation
DD Eligibility if Determined (LOC)
Summary of BDDS Involvement
CMHC Screening
School History and Education (IEP if available)
Psychological testing scores and clinical contact information
Summary of Supports Provided by MR/DD provider &/or CMHC
Child/Youth Referrals
Immunization records
School History & Education, Records & IEP (psychoeducational evaluation, if possible)
History of Past Treatment
Birth Certificate
An updated Admission Referral Form must be submitted for a consumer exceeding 30 days on the admissions
wait list. .
Updates must be submitted by using designated Attachments A or B. A discharge summary from
the current placement must be submitted with the final update. This is to insure that the state hospitals have
current information at admission. Initial referral and referral updates must be discussed and signed by the
consumer &/or legal guardian. A witness must sign for those without legal guardians and/or those refusing to
sign.
Upon admission a written update is required designating behavioral status. A medication reconciliation sheet
must be attached identifying medications given in the last 24-hours, time of next dosage, and a contact number
if SOF needs clarification or further details.
Reference: 1) DMHA Assessment Requirements for Children and Adu lts Entering All State Owned or Operated Mental Health Institutions
2) Definitions of Referral Source to Gatekeeper

DEFINITIONS OF REFERRAL SOURCE TO GATEKEEPER
IMPORTANT: This field identifies who referred the patient to the community mental health center
(CMHC):
(01) Self, family or friend
Client came directly to the CMHC from home, family, streets, etc.
(02) Community Mental Health Center / Managed Care Provider
Client was already the CMHC's patient; or in a group home, halfway house, supervised apartments
Client was referred to the gatekeeper by another CMHC/MCP
(03) Acute Care Hospital
Any inpatient unit other than the CMHC or subcontracted facility or ER
(04) Internal Inpatient Transfer
Transfer from a hospital inpatient unit at the same facility resulting in a separate claim to the payer
source
(05) Human Services Agency
Referral from a social service agency such as shelters, food pantry, and/or non-mental health
related “help” organization
(06) Non-Health Care Facility
Residential service provider not associated with the CMHC
Outpatient service provider not associated with the CMHC
(07) Skilled Nursing or Intermediate Care Facility
Nursing homes and/or rehabilitation centers
(08) Health/Rehab Clinic
Inpatient rehabilitation unit for medical issues and/or critical access hospitals
Assisted living programs
(09) Justice System – Jail, Correctional Facility, Correction-Related Agencies
Office of General Counsel (DMHA legal office) referrals made to SOF’s
Client was referred to the CMHC by police, court, correction/probation agencies, juvenile justice,
probate court, civil court, others.
(10) Information Unavailable
Origin of client’s referral to the CMHC is unavailable or unknown.
Written or verbal history is unable to be verified or determined.
(11) Other Clinic
A free-standing psychiatric provider
Rural health care clinics



