Fillable Printable Health Insurance Application/Change Form
Fillable Printable Health Insurance Application/Change Form
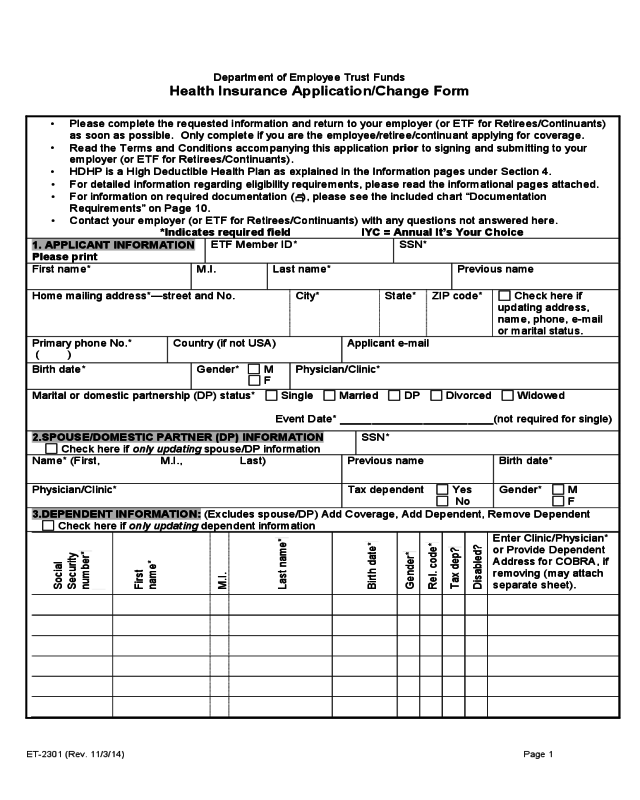
Health Insurance Application/Change Form
Department of Employee Trust Funds
Health Insurance Application/Change Form
•
Please complete the requested information and return to your employer (or ETF for Retirees/Continuants)
as soon as possible. Only complete if you are the employee/retiree/continuant applying for coverage.
•
Read the Terms and Conditions accompanying this application prior to signing and submitting to your
employer (or ETF for Retirees/Continuants).
•
HDHP is a High Deductible Health Plan as explained in the Information pages under Section 4.
•
For detailed information regarding eligibility requirements, please read the informational pages attached.
•
For information on required documentation (
), please see the included chart “Documentation
Requirements” on Page 10.
•
Contact your employer (or ETF for Retirees/Continuants) with any questions not answered here.
*Indicates required field IYC = Annual It’s Your Choice
1. APPLICANT INFORMATION
Please print
ETF Member ID* SSN*
First name* M.I. Last name* Previous name
Home mailing address*—street and No. City* State* ZIP code* Check here if
updating address,
name, phone, e-mail
or marital status.
Primary phone No.*
( )
Country (if not USA) Applicant e-mail
Birth date* Gender*
M
F
Physician/Clinic*
Marital or domestic partnership (DP) status* Single Married DP Divorced Widowed
Event Date* ________________________(not required for single)
2.SPOUSE/DOMESTIC PARTNER (DP) INFORMATION
Check here if only updating spouse/DP information
SSN*
Name* (First, M.I., Last) Previous name Birth date*
Physician/Clinic* Tax dependent Yes
No
Gender* M
F
3.DEPENDENT INFORMATION: (Excludes spouse/DP) Add Coverage, Add Dependent, Remove Dependent
Check here if only updating dependent information
Social
Security
number*
First
name*
M.I.
Last name*
Birth date*
Gender*
Rel. code*
Tax dep?
Disabled?
Enter Clinic/Physician*
or Provide Dependent
Address for COBRA, if
removing (may attach
separate sheet).
ET-2301 (Rev. 11/3/14) Page 1
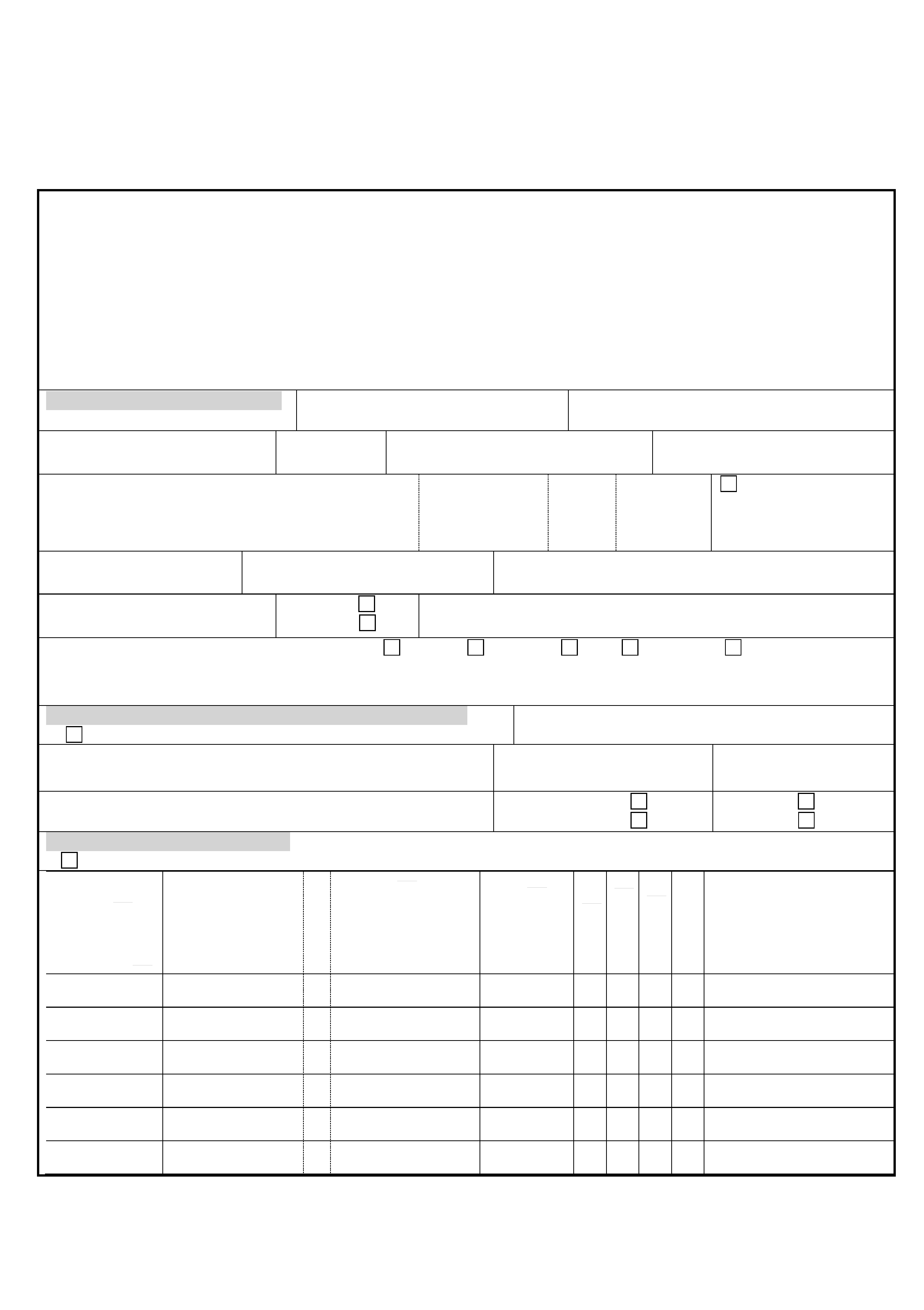
MID_____________________ SSN______________________
4.ENROLLMENT
INFORMATION
New Hire or Return from Leave and Coverage has Lapsed—I want my coverage to
be effective:
When employer contributes to premiums I Decline/Waive Coverage
As soon as possible (employee will pay entire I Decline coverage because I
monthly premium until eligible for employer have other coverage
contribution)
Eligibility reason* Employee Graduate assistant Continuant (COBRA) Retired Survivor
Coverage desired*
Single
Family
Are you
selecting an
HDHP health
plan?
Yes No
Health plan selected*
(enter plan name)
5.REASON FOR APPLICATION*
Please select the event that allows you to enroll outside of initial hire. Reasons marked with
require supporting
documentation. See Page 10 for required documentation listing. IYC = Annual It’s Your Choice
Add Coverage
Spouse/DP to spouse/DP transfer
Transfer from one employer to
another employer
Previous Employer*___________
HIPAA (birth, adoption
, marriage,
DP
, divorce
)
LTE new hire (state only)
Loss of Other Coverage/Employer
Contributions
IYC (eff. Jan. 1)
COBRA (ET-2311 required)
State retiree re-enroll
Effective date* ______________
Other ______________________
Event date* ____________________
Add dependent
HIPAA (birth, adoption
,
marriage, DP
, divorce
)
National medical support
notice
Paternity acknowledgment
Legal ward/guardianship
Eligible dependent not
on initial enrollment
(excludes DP and adult
dependents)
Loss of other coverage/
employer contributions
Disabled, age 26+
IYC (eff. Jan. 1)
Other ___________________
Event date* ________________
Remove dependent
Divorce
/DP terminated
Death of dependent
Legal ward/guardianship ends
Disabled dependent: Disability
ends or support and maintenance
less than 50%.
Grandchild’s parent turns age 18
Adult dependent eligible for other
coverage
IYC (eff. Jan 1)
Other _____________________
Event date* __________________
Change Health Plan (Check one box below, enter new county for a move from service area, indicate current
health plan, provide date of event, update Section 1, if applicable.)
Move from service area Eligible Status Change
Annual IYC (Jan.1)
Status Change event*: _____________________
New county* Current health plan* Event date*_____________
Family to Single Coverage: If your employee premium share is taken pre-tax, IRC Section 125 restricts midyear
changes to your coverage.
My employee-required premium contribution is deducted: (Check one box, list event date and update Section 1.)
Pre-tax and my employee premium contribution has increased significantly
Pre-tax eligible Status Change event
: Event ______________________
Pre-tax change to single during annual It’s Your Choice (Jan. 1)
Post-tax (midyear changes to coverage level can be made at any time)
Event date*______________________________________________
For more information on IRC
Section 125 limitations, see
the Information Pages Section
5 attached to this application
If adding or removing
dependents, please list them in
Section 3.
If removing dependents, please
list their address in Section 3 if
it is different from your own.
Status Change events may include birth, adoption, marriage, creation of DP, divorce or termination of DP.
State and some WPE employees (see
your employer) may select the HDHP
(High Deductible Health Plan) as explained
in the Information Pages Section 4.
ET-2301 (Rev. 11/3/14) Page 2
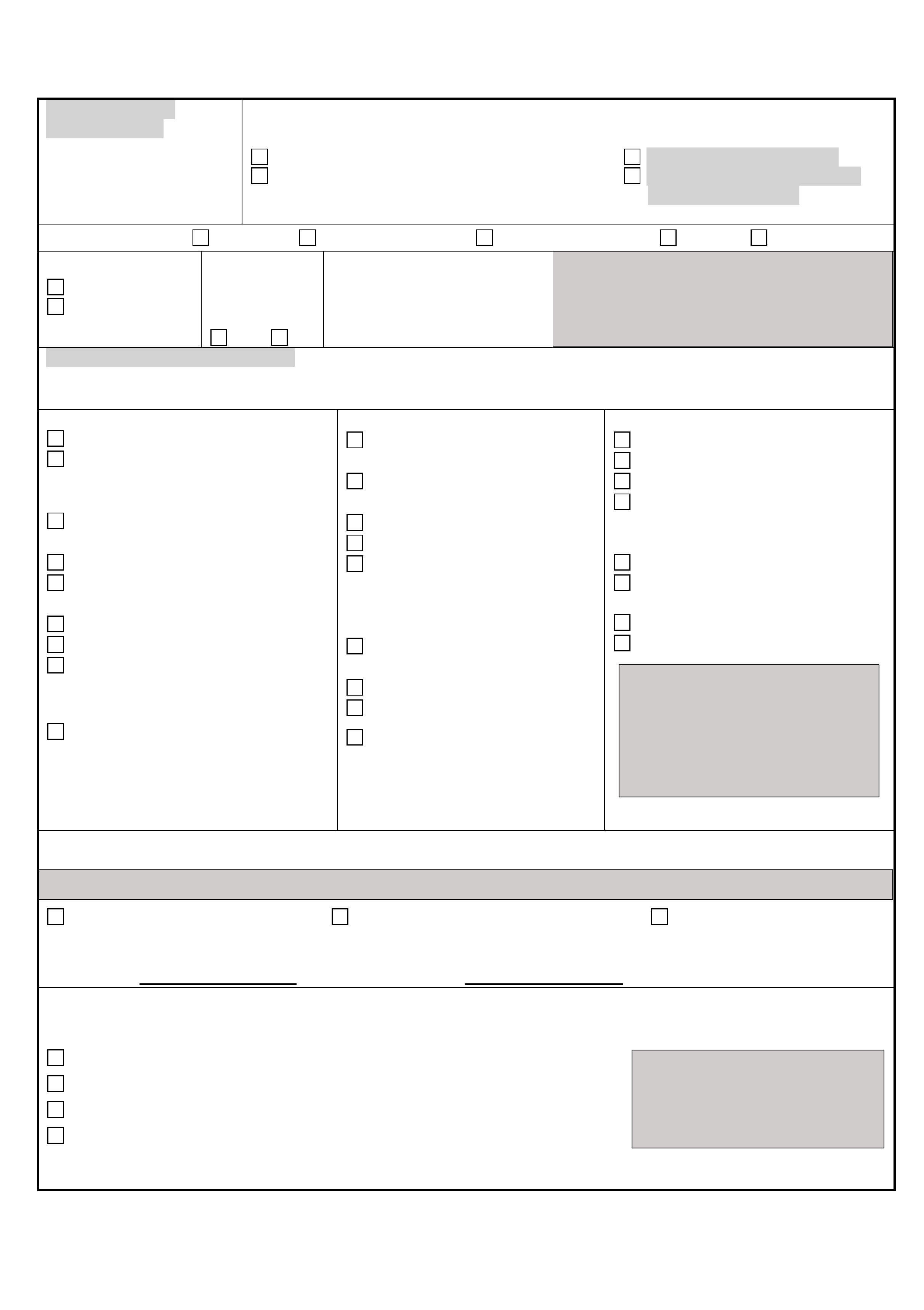
MID_____________________ SSN______________________
Cancel Coverage – If your premiums are deducted on a post-tax basis, you may cancel coverage at any time. If
they are deducted on a pre-tax basis, you must provide the event allowing midyear cancellation. If transfering
family coverage to your spouse/DP, please indicate the IRC Section 125 Status Change Event below.
Retiree sick leave depleted—effective end date of coverage ____________________
My Premiums are Deducted:
Pre-tax (select an event below)
Post-tax (no event required)
I am terminating employment I and all eligible dependents became eligible for
I am going on unpaid leave of absence and enrolled in other coverage
My employee premium share has increased significantly
Spouse/DP to Spouse/DP Transfer
Annual It’s Your Choice Enrollment (Jan. 1)
Status Change Event* ____________________
Additional Information* Is any dependent listed under Section 3 your or your spouse/DP’s grandchild?
No Yes If yes, name of parent_______________________________________________________
Medicare Information/Update Medicare Information*
Are you or any person you insure, covered by Medicare?
No Yes
If yes, list the eligibility reason, names of insured and Medicare Parts A and B effective dates.
Medicare eligible reason: Age Disabled End stage renal disease
Name:___________________ HIC# ___________________ Dates: Part A___________ Part B____________
Name:___________________ HIC# ___________________ Dates: Part A___________ Part B____________
Other Health Insurance Coverage/Update* (State employees are ineligible for HDHP if they have other coverage.)
Do you or any of your dependents have other medical or health care Flexible Spending Account coverage that has
a balance available as of the effective date of this coverage? (excludes dental or vision)
No Yes If yes, complete the following.
Name of company______________________ Policy No. __________________ Group No. ________________
Name(s) of Insured:__________________________________________________________________________
6.SIGNATURE* (Read the Terms and Conditions on Page 4 and sign and date the application.)
By signing this application, I apply for the insurance under the indicated health insurance contract made available
to me through the state of Wisconsin and I have read and agreed to the Terms and Conditions. A copy of this
application is considered as valid as the original. In addition, to the best of my knowledge, all statements and
answers in this application are complete and true. Providing false information is punishable under Wis. Stat.
§943.395. Additional documentation may be required by ETF at any time to verify eligibility.
Sign and date Here & Date Signed (mm/dd/yy)
return to employer (ETF
for Retirees/Continuants) _______________________________________ ___________________
7.EMPLOYER COMPLETES (Coding instructions are in the Employer Health Insurance Administration Manual.)
EIN 69-036- Employer name Payroll representative e-mail
Group number
Employee
type
Coverage
code
Health plan name/suffix
Employment status: Full time Part time LTE Employee deductions: Pre-tax Post-tax
Previous service – complete information
1. Are you a WRS participating employer? Yes No (If yes, answer remaining questions)
2. Previous service check completed? Yes No
3. Did employee participate in the WRS prior to being hired by you? Yes No
4. Source of previous service check? Online Network for Employers (ONE) ETF
Date WRS eligible employment or
graduate appointment began or hire
date
Employer received
date
Event date Prospective coverage date
Payroll representative signature Phone number
( )
ET-2301 (Rev. 11/3/14) Page 3

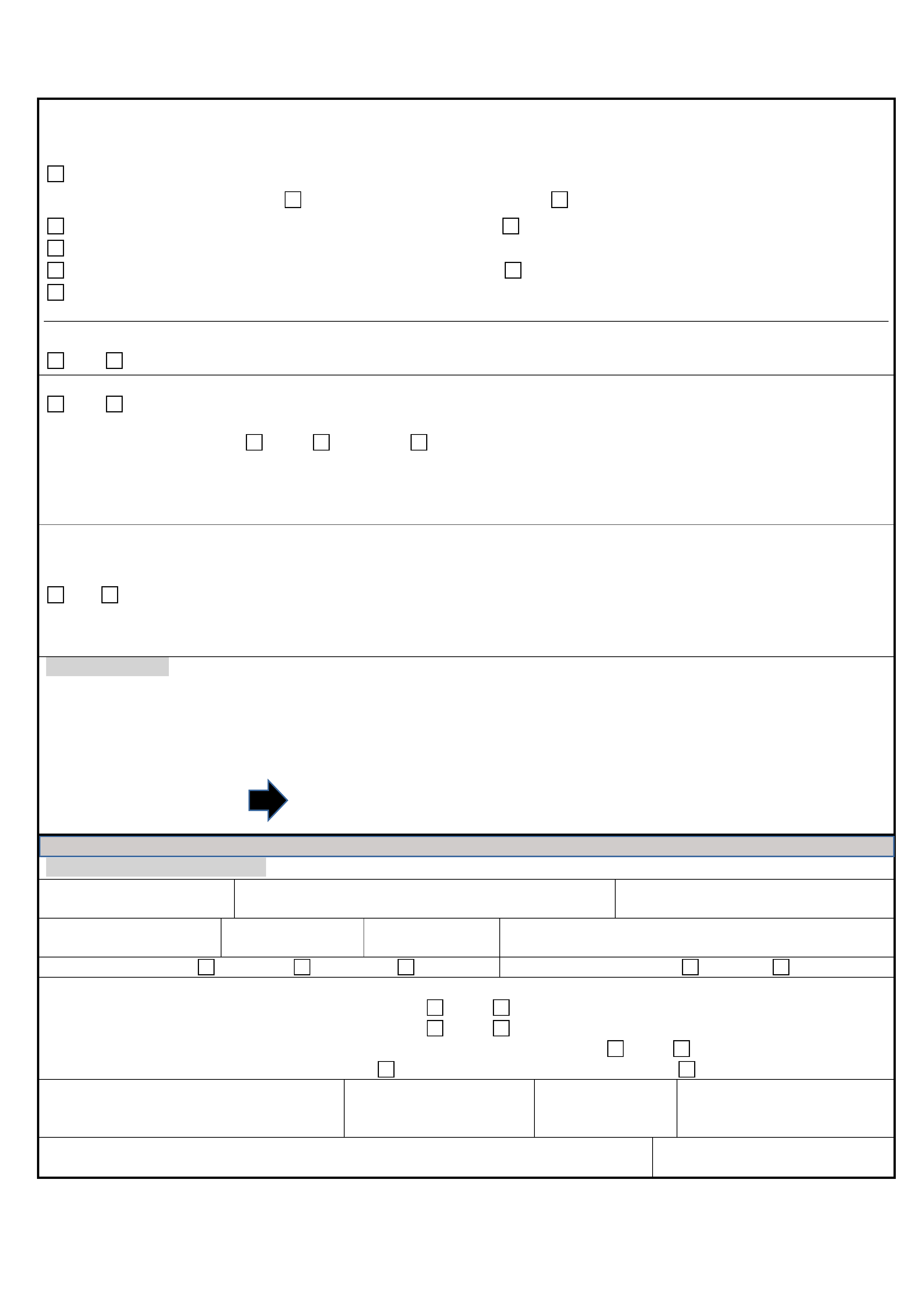
MID_____________________ SSN______________________
TERMS AND CONDITIONS
1. To the best of my knowledge, all statements and answers in this application are complete and true. I understand that if I provide
false or fraudulent information, misrepresentation or fail to provide complete or timely information on this application, I may face
action, including, but not limited to, loss of coverage, employment action, and/or criminal charges/sanctions under Wis. Stat. §
943.395.
2. I authorize the Department of Employee Trust Funds (ETF) to obtain any information from any source necessary to administer
this insurance.
3. I agree to pay in advance the current premium for this insurance, and I authorize my employer (the remitting agent) to deduct
from my wages or salary an amount sufficient to provide for regular premium payments that are not otherwise contributed. The
remitting agent shall send the premium on my behalf to ETF.
4. I understand that eligibility for benefits may be conditioned upon my willingness to provide written authorization permitting my
health plan and/or ETF to obtain medical records from health care providers who have treated me or any dependent(s). If
medical records are needed, my health plan and/or ETF will provide me with an authorization form. I agree to respond to
questions from health plans and ETF, including, but not limited to, audits, in a timely manner.
5. I have reviewed and understand the eligibility criteria for dependents under this coverage and affirm that all listed dependents are
eligible. I understand that children may be covered through the end of the month they turn 26. Children may also be covered
beyond age 26 if they:
• have a disability of long standing duration, are dependent on me or the other parent for at least 50% of support and
maintenance, and are incapable of self-support; or
•
are full-time students and were called to federal active duty when they were under the age of 27 years and while they were
attending, on a full-time basis, an institution of higher education.
6. I understand that if my insured domestic partner and/or dependent child(ren) of my insured domestic partner are not considered
“tax dependents” under federal law, my income will include the fair market value of the health insurance benefits provided to my
domestic partner and/or domestic partner’s dependent child(ren). Furthermore, I understand this may affect my taxable income
and increase my tax liability.
7. I understand that it is my responsibility to notify the employer, or if I am a retiree or continuant to notify ETF, if there is a change
affecting my coverage, including but not limited to, a change in eligibility due to divorce, marriage or domestic partnership, a
change in the “tax dependent” status of my domestic partner and/or domestic partner’s dependent children, or an address
change due to a residential move. Furthermore, failure to provide timely notice may result in loss of coverage, delay in payment
of claims, loss of continuation rights and/or liability for claims paid in error. Upon request, I agree to provide any documentation
that ETF deems necessary to substantiate my eligibility or that of my dependent(s).
8. I understand that if there is a qualifying event in which a qualified beneficiary (me or any dependent(s)) ceases to be covered
under this program, the beneficiary(ies) may elect to continue group coverage as permitted by state or federal law for a maximum
of 18, 29, or 36 months, depending on the type of qualifying event, from the date of the qualifying event or the date of the notice
from my employer, whichever is later. I also understand that if continuation coverage is elected by the affected qualified
beneficiary(ies) and there is a second qualifying event (i.e, loss of eligibility for coverage due to death, divorce, marriage but not
including non-payment of premium) or a change in disability status as determined by the Social Security Administration,
continuation coverage, if elected subsequent to the second qualifying event, will not extend beyond the maximum of the initial
months of continuation coverage. I understand that timely notification of these qualifying events must be made to ETF.
9. I understand that if I am declining enrollment for myself or my dependent(s) (including spouse or domestic partner) because of
other health insurance coverage, I may be able to enroll myself and my dependent(s) in this plan if I or my dependent(s) lose
eligibility for that other coverage (or if the employer stops contributing toward that other coverage). However, I must request
enrollment within 30 days after my or my dependents’ other coverage ends (or after the employer stops contributing toward the
other coverage). In addition, if I have (a) new dependent(s) as a result of marriage, domestic partnership, birth,
acknowledgement of paternity, adoption, or placement for adoption, I may be able to enroll myself and my dependent(s) if I
request enrollment within 30 days after the marriage or effective date of the domestic partnership, or within 60 days after the
birth, acknowledgement of paternity, adoption, or placement for adoption. To request special enrollment or obtain more
information, I should contact my employer (or ETF if I am a retiree or continuant).
10. I understand that I am responsible for enrolling in Medicare Parts A and B when I am first eligible and required by this coverage,
and that as the subscriber I am responsible for ensuring my spouse, domestic partner and any other eligible dependents also
enroll in Medicare Parts A and B when they are first eligible, to ensure proper coordination of benefits with Medicare. In the
event I or any eligible dependent does not enroll in Medicare Parts A and B when first eligible and required by this group health
insurance program, I understand that I will be financially liable for the portion of claims Medicare would have paid had proper
Medicare enrollment been attained.
11. I agree to abide by the terms of my benefit plan, as explained in any written materials I receive from ETF or my health plan,
including, without limitation, the It’s Your Choice guides.
ET-2301 (Rev. 11/3/14) Page 4

Information Pages
Initial Eligibility
You must enroll online through myETF Benefits or submit this application to your employer if you are
actively employed, or to the Department of Employee Trust Funds if you are a retiree or on
continuation. Your initial enrollment period is as follows:
a) Within 30 days of your date of hire to be effective the first of the month on or following receipt
of application by the employer; or
b)
Active State Employees only – Before becoming eligible for state employer contributions
(completion of two months of state service under the Wisconsin Retirement System for
permanent or project employees). Limited Term Employees (LTE) must complete six months
of state service to be eligible for employer contributions. Employees of WISCRAFT must
complete 1,000 hours of service to be eligible for employer contributions. This does not apply
to UW unclassified faculty/academic staff.
c)
Wisconsin Public Employers’ participants only – Within 30 days prior to becoming eligible
for employer contribution as determined by your employer, not to exceed six months.
d)
Graduate Assistants only – When you are notified of your appointment, immediately contact
your benefits/payroll/personnel office for health insurance enrollment information and an
application. If eligible, you may enroll for single or family coverage in any of the available
health plans. Your benefits/payroll/personnel office must receive your application within 30
days of the date of your first eligible appointment. Your health insurance coverage will be
effective the first day of the month on or following receipt of your application by your
employer.
If this is not your first eligible appointment, you may still be eligible for the initial 30-day
enrollment period if you had a 30-day employment break in service between appointments. If
you are currently or later become an active participant under the WRS, you will not be eligible
for coverage under the graduate assistant program as a WRS participant.
e)
Retirees only – Health insurance continues automatically upon retirement. To change or
cancel your existing coverage during the open enrollment period, complete this application or
go online to myETF Benefits at myetf.wi.gov/ETFmMEBWeb/mMEB/mMEBLogon.jsp
.
Changes become effective the first of the year and cancellations are effective the end of the
month in which they are received or a future end of the month if specified. Cancellations
cannot be back-dated but can be done at any time of the year by mailing or faxing a signed
request to ETF - Retiree Services Section.
If you choose to enroll within your initial enrollment period, we recommend that you submit this
application to your employer immediately upon employment. If you missed your enrollment
opportunity there may be other enrollment opportunities available. There are no interim effective
dates, except as required by federal HIPAA law. If your application is submitted after these
enrollment opportunities, you will not be eligible to enroll until the annual It’s Your Choice Open
Enrollment period. For complete enrollment and program information, read the It’s Your Choice
Decision and Reference guides.
ET-2301 (Rev. 11/3/14) Page 5

Information Pages
1. Applicant Information
Please provide the information requested in this section as completely as possible. Please provide
physician/clinic information unless you have selected WPS/Standard Plan as your health plan.
Please provide your care system if you have selected WEA Trust NW as your health plan.
Include your e-mail address if you would like ETF to contact you by e-mail if we need to request
information related to your health coverage.
Indicate your marital status and date (single does not require a date). The effective date of a DP is
the date that ETF receives the Affidavit of Domestic Partnership (ET-2371) form; your health
application must be received within 30 days of this date if you also wish to provide health coverage
for your domestic partner (DP). If you are divorced, the entry of judgment of divorce is typically when
the judge signs the divorce decree and the clerk of courts date stamps the decree.
Personal Data Update/Correction: Please check the update box under Section 1, 2, or 3 if you are
only updating demographic information (address, SSN, birth date, marital status, gender, phone or e-
mail) for yourself, your spouse/DP, or your dependents.
2. Spouse/Domestic Partner (DP) Information
The Centers for Medicare and Medicaid Services (CMS) require that ETF report the name, SSN, birth
date, and prior name, if any, for your spouse or DP, even if they are not covered on your health
insurance. If you indicate your marital status is married or DP, you must provide this information even
if you elect single coverage. If you do not file an Affidavit of Domestic Partnership (ET-2371) form
with ETF, then you are not in a domestic partnership for purposes of health insurance, and this
information is not required for your DP. If you apply for family coverage, please also provide gender,
tax dependent status (yes or no) and physician/clinic (required for all covered individuals). If you
select WEA Trust NW, you must select a care system. Exception: you do not need to select a
physician/clinic or care system if you have elected the Standard Plan/WPS.
3. Dependent Information
If you are covering dependents other than your spouse/DP or are updating information for a currently
covered dependent in the Personal Data Update/Correction Section, please provide the information
requested.
For Rel. Code, use the following codes to describe the relationship of dependents to you:
01=Spouse 24=Dependent of Minor Dependent
15=Legal Ward 53=Domestic Partner
17=Stepchild 38=Dependent of Domestic Partner
19=Child
03=Minor Parent of Minor Dependent (This relationship is a Legal Ward, Stepchild, Child, or
Dependent of DP who is younger than age 18 and is the parent of any of your or your spouse’s/DP's
grandchildren listed as an eligible dependent on this application. Grandchildren cannot be covered on
your contract unless the parent of the grandchild is covered and is younger than age 18.)
Indicate “Yes” or “No” if any dependent older than age 26 is disabled.
Indicate “Yes” or “No” if your DP/dependent of DP is considered a “tax dependent” under federal law.
If removing adult dependents, list their address in this section if it is different from your own.
ET-2301 (Rev. 11/3/14) Page 6

Information Pages
4. Enrollment Information
New Hire Only: If you are a newly hired employee, please indicate when you want coverage to start:
1) immediately (as soon as possible) or 2) when you become eligible for the employer contribution
toward the health insurance premium. Coverage will be effective the first of the month following receipt
of the application or eligibility for the employer contribution. If you do not wish to enroll, please mark if
you: 1) decline/waive coverage or 2) decline coverage because you have other coverage.
Eligibility Reason: Please indicate your eligibility reason by indicating if you are an employee,
graduate assistant, COBRA continuant, surviving dependent of a covered employee or you are
retired and receiving an annuity.
A High Deductible Health Plan (HDHP) has a minimum annual deductible and a maximum annual
out-of-pocket limit. An HDHP generally begins paying for health care costs once the annual
deductible has been met. Preventive services mandated by federal law are not subject to the annual
deductible. For more information, please see the It’s Your Choice 2015 Decision and Reference
guides. If you are unsure if you are enrolling in an HDHP, please contact your employer or ETF.
For state employees, you may not select an HDHP if you are enrolled in a health care Flexible
Spending Account or Employee Reimbursement Account that has a balance available as of the
effective date of this coverage, even if you have a qualifying HIPAA event during the plan year.
Coverage Desired: Indicate if you wish to have single coverage (for yourself only), family coverage
(yourself and all eligible dependents), HDHP single coverage (for yourself only), or HDHP family
coverage.
Health Plan Selected: Indicate which health plan you wish to provide your health insurance. A listing
of health plans available is located in the It’s Your Choice Decision Guide.
5. Reason for Application
Indicate if you are using this application to Add Coverage (other than if you are a New Hire), Add
Dependent(s), Remove Dependent(s), Change Health Plan, Switch from Family to Single coverage,
or if you are updating or correcting personal data for yourself, spouse/DP, or dependent(s) by
selecting a reason under the appropriate heading.
If the reason is Add Coverage, Add Dependent, or Remove Dependent and none of the reasons
provided suit your situation, please select other and provide the reason as well as the event date if an
event is associated with your reason. This may result in your request being denied if the reason is not
allowed under the contract. Your employer will be notified if this is the case.
When removing a spouse and stepchildren, if any, due to divorce, the entry of judgment of divorce is
typically when the judge signs the divorce decree and the clerk of courts date stamps the decree.
Adult Dependents younger than age 19 cannot be dropped from coverage when family coverage is in
place. Once the dependent turns 19, that adult dependent can be dropped at the end of the calendar
year they turned 19 during the annual It’s Your Choice (IYC) Open Enrollment period. An adult
dependent older than 19 can be dropped or added during any IYC period.
Change Health Plan: Please indicate the event that makes you eligible to change plans, list your
new county if moving from the service area, your current health plan, and the date of the event that
qualified you to make the change.
If you are changing health plan and wish to change coverage level at the same time due to a HIPAA
qualifying event, you must submit two separate applications. The coverage level change will be
effective on the event date and the carrier change will be effective the first of the month following the
receipt of the applications which must be received within 30 days of the event.
For state employees, you may not select an HDHP if you are enrolled in a health care Flexible
Spending Account or Employee Reimbursement Account, even if you have a qualifying HIPAA event
during the plan year.
ET-2301 (Rev. 11/3/14) Page 7
Information Pages
Family to Single Coverage: To make a change from family to single coverage other than during
annual IYC, you must qualify to do so under one of the reasons provided if your health insurance
premiums are deducted pre-tax. Please select a reason from the list and provide an event date. If
your deductions are taken post-tax, please check the post-tax box.
Retiree premiums are deducted on a post-tax basis and a change from Family to Single Coverage
may be done at any time by submitting this form or by applying online through myETF Benefits at
myetf.wi.gov/ETFmMEBWeb/mMEB/mMEBLogon.jsp. The change will be effective the first of the
month following receipt of your paper or online application.
Internal Revenue Code (IRC) Section 125: If you are enrolled in a Section 125 plan for premium
conversion, medical or dependent day care coverage, then section 125 may limit your ability to make
some changes to your coverage, for example, it will prevent you from canceling coverage at any time
unless you have a change of status event. For the most part, these change of status events
correspond to HIPAA qualifying events, but in certain circumstances we will need to ask you to state
the section 125 change of status event you fall under.
Cancel Coverage: Please indicate if your health insurance premiums are deducted pre-tax or post-
tax. If you are unsure, your human resources person should be able to tell you. After indicating the
tax status of your premiums, please select a reason for your cancellation and provide the change in
status event that is allowing the cancellation if you are cancelling under IRC Section 125.
Cancellation is effective the end of the month on or following receipt of the application by ETF.
Retirees pay premiums post-tax and do not need to provide a reason for cancellation. If you wish to
cancel on a future date, please provide that date on the line provided under Cancel Coverage.
Otherwise, coverage will end at the end of the month following receipt of your request.
Additional Information: Indicate “Yes” or “No” and list the name of your or your spouse/DP’s
grandchild’s parent.
Medicare Information/Update Medicare Information: Indicate “Yes” or “No” if you or any of your
dependents (including your spouse/DP) are covered by Medicare, and list their names. Provide the
Medicare eligibility reason, Health Insurance Claim Number (HIC#), and date(s) Medicare Part A
and/or Part B are effective. This information can be found on the Medicare card of the Medicare
eligible person. Please send a copy of the Medicare card and the Medicare Eligibility Statement
(ET-4307) to ETF.
If you are an active employee and your age 65 or older domestic partner is covered on your
insurance, they must be enrolled in Medicare parts A and B. Medicare will be the primary payer for
your Medicare eligible domestic partner’s medical expenses.
Other Health Insurance Coverage/Update: Please provide any information regarding any other
group health insurance coverage under which you or your dependent(s) (including your spouse/DP)
are covered. For state employees, you are not eligible for the HDHP if you have other health
insurance coverage (including, but not limited to, coverage from a spouse's plan, Medicare,
TRICARE, or a health care Flexible Spending Account or Employee Reimbursement Account).
Note: “Other coverage” does not include supplemental insurance (examples: EPIC or DentalBlue).
For State employees, other coverage does include health care Flexible Spending Accounts or
Employee Reimbursement Accounts for purposes of HDHP eligibility. If you have an available
balance in a health care FSA or ERA as of the effective date of HDHP coverage, then you are
ineligible for HDHP coverage.
During Annual It’s Your Choice, if you are not making any changes to your coverage you do not
need to submit an application.
ET-2301 (Rev. 11/3/14) Page 8

Information Pages
6. SIGNATURE
Your signature is required. Applications without a signature will be rejected.
Read the Terms and Conditions on Page 4 of this application packet. Only after you have read this
should you sign, date, and submit your application to your employer (or to ETF, if you are a retiree or
continuant).
1.
When submitting an application for any reason, you are required to read the Terms and
Conditions on the last page of this application and sign and date the application. By signing
the application, you are acknowledging that you have read and agree to the Terms and
Conditions.
2. Make a copy of the application for your records and submit the original application to your
payroll or benefits representative. If you are a retiree or continuant, please submit your
application directly to ETF.
3. Your employer will complete Section 7 and provide a copy of the application to you. For
retirees or continuants, ETF will complete Section 7 and provide a copy of the application to
you.
ET-2301 (Rev. 11/3/14) Page 9
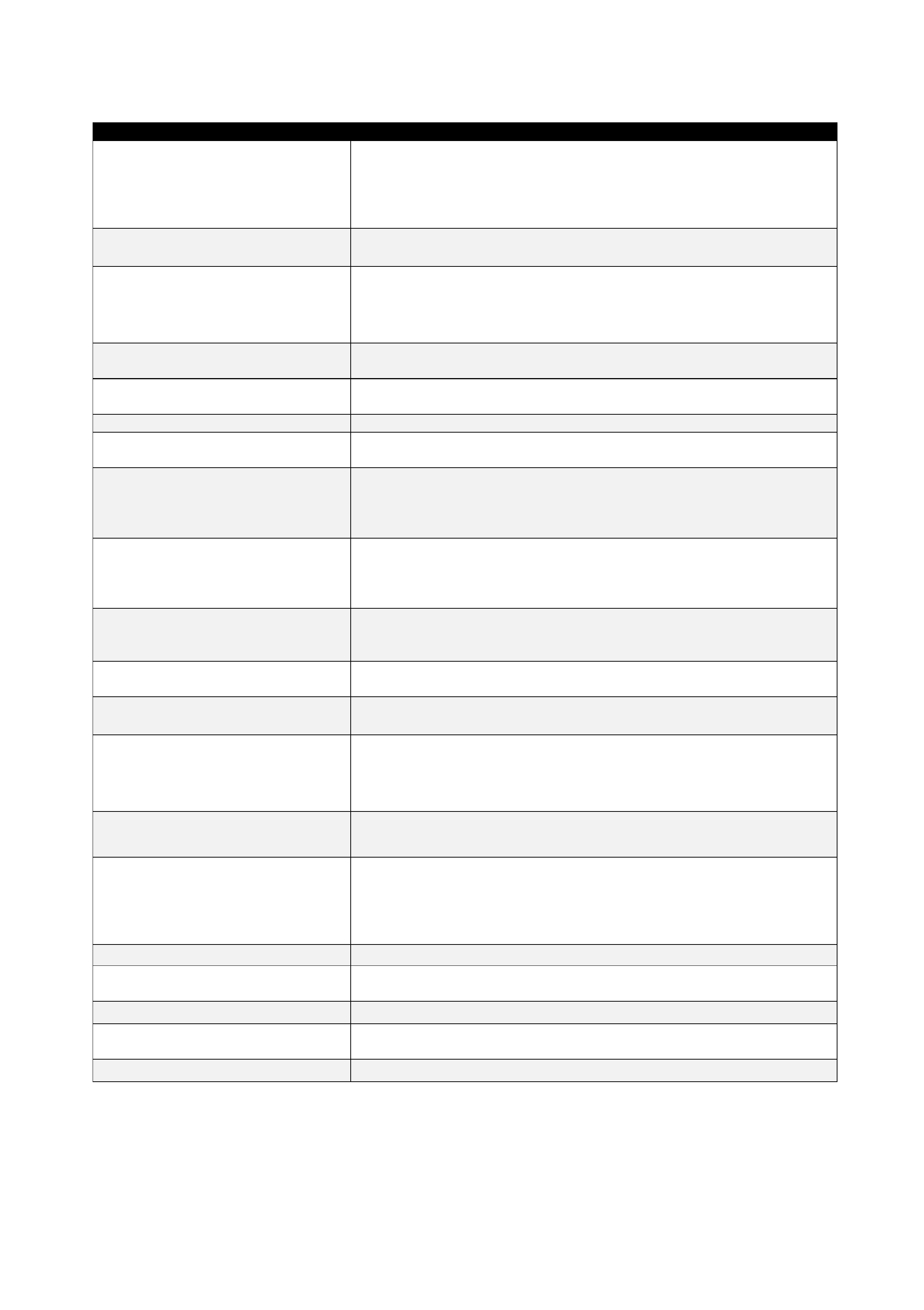
4. Documentation Requirements
Reason for Change or Enrollment Type of Documentation
Loss of Other Coverage
Certificate of Creditable Coverage from health plan; COBRA notice if
coverage end date, covered individuals, and health plan are indicated;
or letter from administrator if self-funded health plan. If loss of
employer premium contributions, letter from employer indicating they
no longer contribute towards their employee’s premium.
Divorce
Family to single
No documents required but ETF may request per the Terms and
Conditions on Page 4 of this application, Number 7.
Divorce
Family coverage remains in place
when more dependents than
spouse/stepchildren covered
Copy of Continuation/Conversion Notice (ET-2311) sent to ex-spouse
of the subscriber (ETF may request copy of divorce decree from clerk
of courts showing date of entry of divorce if needed per the Terms and
Conditions on Page 4 of this application, Number 7).
Adoption Recorded copy of court order granting adoption or letter of placement
for adoption.
Legal Ward
Court Order (Letters of Guardianship) granting permanent
guardianship of person.
National Medical Support Notice Copy of National Medical Support Notice.
Paternity Court order declaring paternity, or Voluntary Paternity
Acknowledgement (HCF-5024) filed w/DHS, or birth certificate.
Creating a domestic partnership
Copy of Acknowledgement Letter (ET-2373) indicating effective date
of domestic partnership submitted to employer by employee. Health
application adding DP should be submitted to employer when Affidavit
of Domestic Partnership (ET-2371) is submitted to ETF.
Cancel coverage due to
enrollment in other health insurance
coverage when premium
contributions are deducted pre-tax
Copy of medical ID card or letter from health plan indicating effective
date of other coverage. Must be received within 30 days of enrollment
in other coverage.**
Family to single because all
dependents enrolled in other
coverage
Same rules as Cancel above.**
Birth
Original birth certificate not required. ETF may request documentation
per the Terms and Conditions on Page 4 of this application, Number 7.
Marriage
Original marriage certificate is not required (ETF may request per the
Terms and Conditions on Page 4 of this application, Number 7).
Ending a domestic partnership
Affidavit of Termination of Domestic Partnership (ET-2372). (ETF
may request copy of marriage certificate if marriage is reason for
termination of domestic partnership per the Terms and Conditions on
Page 4 of this application, Number 7.)
Change of address/telephone
None (ETF may request documentation per the Terms and Conditions
on Page 4 of this application, Number 7.)
Eligible and enrolled in Medicare
Copy of Medicare card and Medicare Eligibility Statement (ET-4307).
(Note: If you are on COBRA Continuation and the subscriber or
dependents become Medicare eligible after the COBRA effective
date, subscriber or dependent(s) is no longer eligible to continue on
COBRA.)
Death Original death certificate.
Legal change of name (other than
due to marriage or divorce)
Copy of court order.
Social Security number change Copy of card or letter from Social Security Administration.
State retiree re-enroll Same as loss of other coverage and an ET-4317. During IYC, no
documentation required.
Disabled, age 26+ Copy of letter from health plan approving disabled status
Documentation Required/Must Be Submitted to ETF.
**Does not apply to retirees.
ET-2301 (Rev. 11/3/14) Page 10



