Fillable Printable Medicare Cost Sharing For Members
Fillable Printable Medicare Cost Sharing For Members
Medicare Cost Sharing For Members

AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 200 - CLAIMS
201 - Page 1 of 8
201 - MEDICARE COST SHARING FOR MEMBERS COVERED BY MEDICARE AND
MEDICAID
EFFECTIVE DATES: 10/01/97, 02/01/13, 07/01/13, 12/01/14, 07/01/16, 09/20/17
REVISION DATES: 06/01/01, 03/11/10, 01/03/13, 06/06/13, 07/18/13, 11/20/14, 05/19/16,
09/07/17
I. PURPOSE
This Policy applies to Acute, ALTCS/EPD, CRS, DCS/CMDP (CMDP), DES/DDD (DDD),
and RBHA Contractors. The purpose of this Policy is to define Contractor cost sharing
responsibilities for members that are Dual-Eligible Medicare Beneficiaries (Duals) receiving
Medicare Parts A and/or B through Original Fee-For-Service (FFS) Medicare or a Medicare
Advantage Plan. The purpose of this Policy is also to maximize cost avoidance efforts by
Managed Care Contractors and to provide a consistent reimbursement methodology for
Medicare cost sharing as outlined in section 1905(p)(3) of the Social Security Act.
II. DEFINITIONS
COST SHARING
The Contractors’ obligation for payment of applicable Medicare
coinsurance, deductible, and copayment amounts for Medicare
Parts A and B covered services.
DUAL ELIGIBLE
MEDICARE
BENEFICIARIES (DUALS)
An AHCCCS member who is eligible for both Medicaid and
Medicare services. There are two types of Dual Eligible
members: QMB Duals and Non-QMB Duals (FBDE, SLMB+,
QMB+)
FULL BENEFIT DUAL
ELIGIBLE (FBDE)
An AHCCCS Member who does not meet the income or
resources criteria for a QMB or an SLMB. Eligible for
Medicaid either categorically or through optional coverage
groups, such as Medically Needy or special income levels for
institutionalized or home and community-based waivers.
IN-NETWORK
PROVIDER
A provider that is contracted with the Contractor to provide
services.
MEDICARE ADVANTAGE
PLAN
A private health insurance plan that has a contract with the
Centers for Medicare and Medicaid Services (CMS) to provide
all Medicare benefits covered under Parts A and B to Medicare
beneficiaries who choose to enroll in their plan. Most plans
include prescription drug coverage and may also provide
additional benefits. Types of Medicare Advantage plans
include Local Health Maintenance Organizations (HMOs),
Special Needs Plans (SNPs), and Local and Regional Preferred
Provider Organizations (RPPOs).

AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 200 - CLAIMS
201 - Page 2 of 8
MEDICARE PART A
Hospital insurance that provides coverage for inpatient care in
hospitals, skilled nursing facilities, and hospice.
MEDICARE PART B
Coverage for medically-necessary services like doctors'
services, outpatient care, home health services, and other
medical services.
MEDICARE PART D
Medicare prescription drug coverage.
NON-QUALIFIED
MEDICARE BENEFICIARY
(NON-QMB) DUAL
A person who qualifies to receive both Medicare and Medicaid
services, but does not qualify for the QMB program as outlined
in A.A.C. R9-29-101.
OUT OF NETWORK
PROVIDER
A provider that is neither contracted with nor authorized by the
Contractor to provide services to its members.
QUALIFIED MEDICARE
BENEFICIARY DUAL
(QMB DUAL)
A person determined eligible under A.A.C. R9-29-101 et seq.
for QMB and eligible for acute care services provided for in
A.A.C. R9-22-201 et seq. or ALTCS services provided for in
A.A.C. R9-28-201 et seq. A QMB dual person receiving both
Medicare and Medicaid services and cost sharing assistance.
QUALIFIED MEDICARE
BENEFICIARY ONLY
(QMB ONLY)
A person who qualifies to receive Medicare services only and
cost-sharing assistance known as QMB.
SPECIFIED LOW-INCOME
MEDICARE BENEFICIARY
(SLMB)
Persons entitled to Medicare Part A whose incomes are between
100-120 per cent of the National Poverty Level. Medicaid also
covers the beneficiary’s Part B premium costs.
SUPPLEMENTAL
BENEFITS
Benefits which may be offered by Medicare Advantage plans
which are not traditionally covered under Medicare Parts A and
B. These benefits may include, but are not limited to,
preventative dental and standard vision benefits.
III. POLICY
For QMB Duals and Non-QMB Duals, the Contractor’s cost sharing payment
responsibilities are dependent upon various factors:
Whether the service is covered by Medicare only, by Medicaid only or by both
Medicare and Medicaid,
Whether the services are received in or out of network (the Contractor only has
responsibility to make payments to AHCCCS registered providers),
Whether the services are emergency services, and/or
Whether the Contractor refers the member out of network.
Refer to sections A-B of this policy and. to A.A.C. Title 9, Chapter 29, Article 3.

AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 200 - CLAIMS
201 - Page 3 of 8
An exception to the Contractor’s cost sharing payment responsibility described below
applies to days in a Skilled Nursing Facility. For stays in a Skilled Nursing Facility, the
Contractor shall pay 100% of the member cost sharing amount for any Medicare Part A
Skilled Nursing Facility (SNF) days (21 through 100) even if the Contractor has a Medicaid
Nursing Facility rate less than the amount paid by Medicare for a Part A SNF day.
For Contractor responsibilities regarding coordination of benefits activities for members
who have third-party coverage other than Medicare, refer to ACOM Policy 434.
A. QMB DUALS
QMB Duals are entitled to all Medicaid and Medicare Part A and B covered services.
These members are identified by a Medicare Part C entry in their AHCCCS Medicare
record and typically by a two in the third digit of the rate code. A QMB Dual eligible
member who receives services under A.A.C.R9-22-2 or A.A.C. R9-28-2
from a
registered provider is not liable for any Medicare copayment, coinsurance or deductible
associated with those services and is not liable for any balance of billed charges. (A.A.C.
R9-29-302)
CONTRACTOR PAYMENT RESPONSIBILITIES
1. The Contractor is responsible for payment of Medicare cost sharing (deductible,
coinsurance, and copayment) amounts for all Medicare Part A and B covered
services, including services not covered by AHCCCS, subject to the limits outlined in
this Policy. See also AMPM Chapter 300, Section 310. These services include:
a. Chiropractic services for adults,
b. Outpatient occupational and speech therapy coverage for adults,
c. Orthotic devices for adults,
d. Cochlear implants for adults,
e. Services by a podiatrist, and
f. Any services covered by or added to the Medicare program not covered by
Medicaid.
2. The Contractor is prohibited from using the 09 coverage code to deny payment for
medically necessary services to members who are both Medicare and Medicaid
eligible. The 09 coverage code is used by AHCCCS to resolve coding discrepancies
between Medicare and Medicaid, and shall not be used to deny payment of claims.
3. The Contractor only has responsibility to make payments to AHCCCS registered
providers.
4. The payment of Medicare cost sharing for QMB Duals must be provided regardless
of whether the provider is in the Contractor's network or prior authorization has been
obtained.
5. The Contractor shall have no cost sharing obligation if the Medicare payment exceeds
the Contractor’s contracted rate for the services. The Contractor’s liability for cost
sharing plus the amount of Medicare’s payment shall not exceed the Contractor’s
AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 200 - CLAIMS
201 - Page 4 of 8
contracted rate for the service. There is no cost sharing obligation if the Contractor
has a contract with the provider, and the provider’s contracted rate includes Medicare
cost sharing. The exception to these limits on payments as noted above is that the
Contractor shall pay 100% of the member copayment amount for any Medicare Part
A SNF days (21 through 100) even if the Contractor has a Medicaid Nursing Facility
rate less than the amount paid by Medicare for a Part A SNF day.
6. In accordance with A.A.C. R9-29-302, unless the subcontract with the provider sets
forth different terms, when the enrolled member (QMB Dual) receives services from
an AHCCCS registered provider in or out of network the following applies (Table 1
and Figure 1):
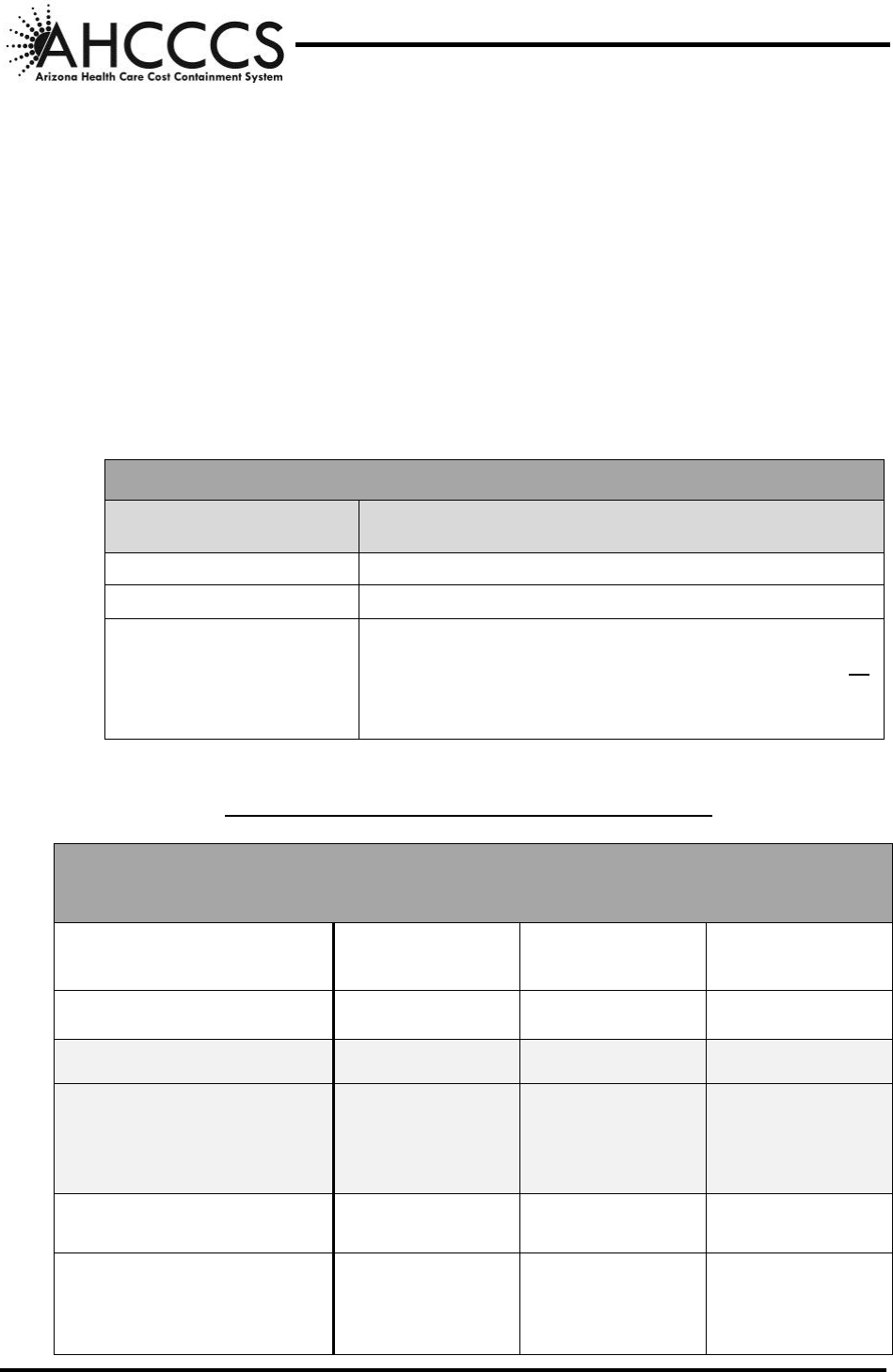
TABLE 1: QMB DUALS
QMB DUALS
WHEN THE SERVICE IS
COVERED BY:
THE CONTRACTOR SHALL PAY
(Subject to the limits outlined in this Policy)
Medicare Only
Medicare copayments, coinsurance and deductible
Medicaid Only
The provider in accordance with the contract
By both Medicare and
Medicaid
(See Examples Below)
The lesser of:
a. The Medicare copay, coinsurance or deductible, or
b. The difference between the Contractor’s contracted
rate and the Medicare paid amount.
FIGURE 1 – QMB DUAL COST SHARING - EXAMPLES
SERVICES ARE COVERED BY BOTH MEDICARE AND MEDICAID
Subject to the limits outlined in this Policy
EXAMPLE 1
(b. In Table 1 above)
EXAMPLE 2
(b. In Tab le 1 above)
EXAMPLE 3
(b. In Table 1 above)
Provider charges
$125
$125
$125
Medicare rate for service
$100
$100
$100
Medicaid rate for Medicare
service (Contractor’s
contracted rate)
$100
$90
$90
Medicare deductible
$0
$0
$40
Medicare paid amount (80%
of Medicare rate less
deductible)
$80
$80
$40
AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 200 - CLAIMS
201 - Page 5 of 8
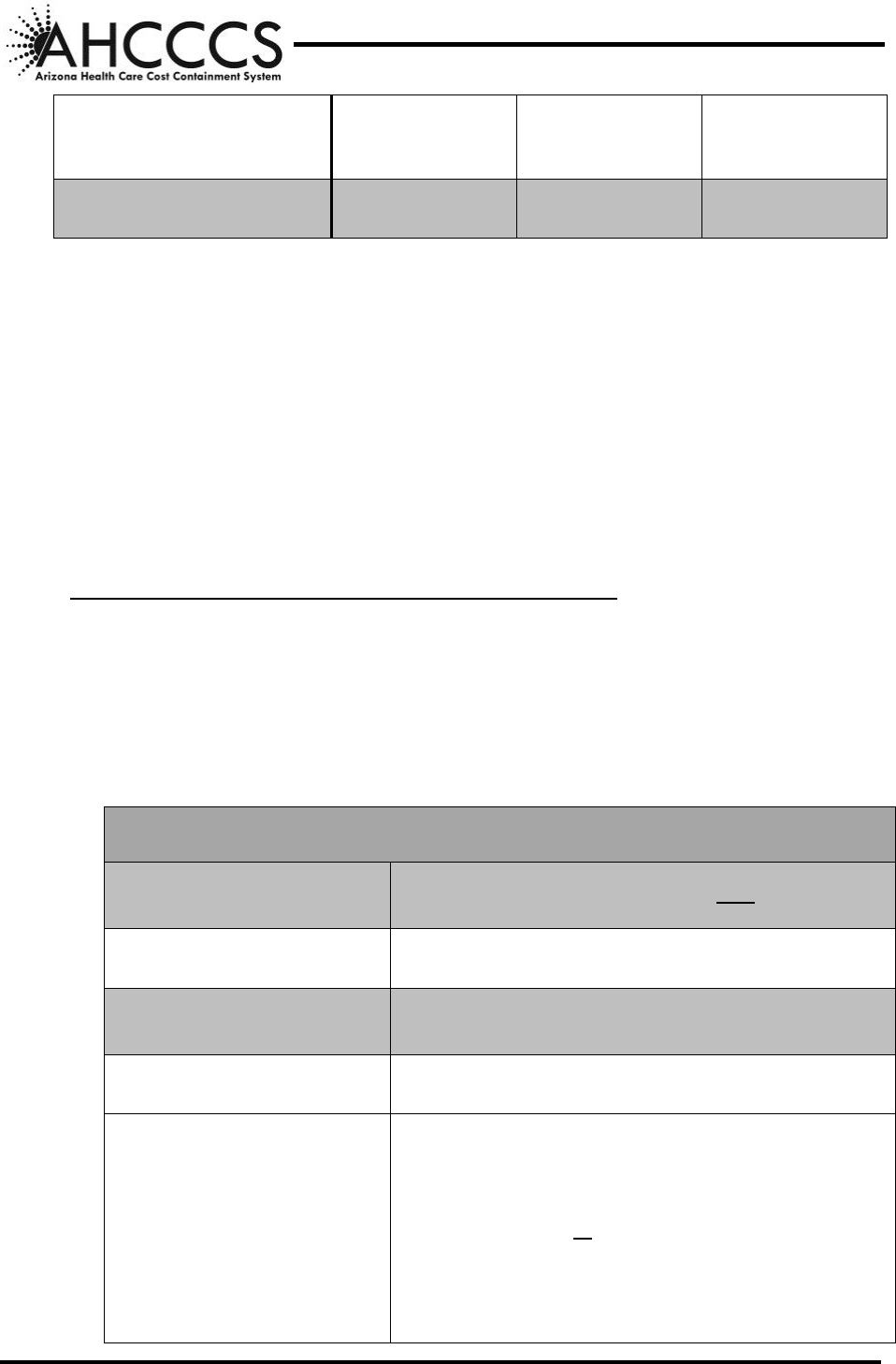
Medicare coinsurance (20%
of Medicare rate)
$20
$20
$20
CONTRACTOR PAYS
$20
$10
$50
B. NON-QMB DUALS
A Non-QMB Dual eligible member who receives covered services under 9 A.A.C. 22,
Article 2 or 9, 9 A.A.C. 28, Article 2 from a provider within the Contractor's network is
not liable for any Medicare copay, coinsurance or deductible associated with those
services and is not liable for any balance of billed charges unless services have reached
the limitations described within A.A.C. R9-22, Article 2. When the Non-QMB Dual
Member elects to receive services out of network that are covered by both Medicare and
Medicaid, the member is responsible for any Medicare copay, coinsurance or deductible
unless the service is emergent, or, for non-emergency services, the provider has obtained
the member’s approval for payment as required in A.A.C. R9-22-702.
CONTRACTOR PAYMENT RESPONSIBILITIES (IN NETWORK)
1. In accordance with A.A.C. R9-29-303, when an enrolled member (Non-QMB Dual)
receives services within the network of contracted providers and the service is
covered up to the limitations described within A.A.C. R9-22-2, the member is not
liable for any balance of billed charges and the following applies (Table 2):
TABLE 2: NON-QMB DUALS (IN NETWORK)
NON-QMB DUALS (IN NETWORK)
WHEN THE SERVICE IS
COVERED BY:
THE CONTRACTOR SHALL NOT PAY:
Medicare Only
Medicare copay, coinsurance or deductible
WHEN THE SERVICE IS
COVERED BY:
THE CONTRACTOR SHALL PAY:
(SUBJECT TO THE LIMITS OUTLINED IN THIS POLICY)
Medicaid Only
The provider in accordance with the contract
By both Medicare and
Medicaid
The lesser of the following (unless the subcontract with
the provider sets forth different terms):
a. The Medicare copay, coinsurance or deductible,
or
b. Any amount remaining after the Medicare paid
amount is deducted from the subcontracted rate
(Contractor’s contracted rate).
AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 200 - CLAIMS
201 - Page 6 of 8
CONTRACTOR PAYMENT RESPONSIBILITIES (OUT OF NETWORK)
2. In accordance with A.A.C. R9-29-303, when an enrolled member (Non-QMB Dual)
receives services from a non-contracting provider the following applies (Table 3):
TABLE 3: NON-QMB DUALS (OUT OF NETWORK)
NON-QMB DUALS (OUT OF NETWORK)
WHEN THE SERVICE IS
COVERED BY:
THE CONTRACTOR
Subject to the limits outlined in this Policy
Medicare Only
Has no responsibility for payment.
Medicaid only and the
Contractor has not referred the
member to the provider or has
not authorized the provider to
render services and the services
are not emergent
Has no responsibility for payment.
Medicaid only and the
Contractor has referred the
member to the provider or has
authorized the provider to
render services or the services
are emergent
Shall pay in accordance with A.A.C. R9-22-705.
By both Medicare and Medicaid
and the Contractor has not
referred the member to the
provider or has not authorized
the provider to render services
and the services are not
emergent
Has no responsibility for payment.
By both Medicare and Medicaid
and the Contractor has referred
the member to the provider or
has authorized the provider to
render services or the services
are emergent
Shall pay the lesser of:
a. The Medicare copay, coinsurance or
deductible, or
b. Any amount remaining after the Medicare
paid amount is deducted from the amount
otherwise payable under A.A.C. R9-22-705.

AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 200 - CLAIMS
201 - Page 7 of 8
C. PRIOR AUTHORIZATION
The Contractor can require prior authorization. If the Medicare provider determines that
a service is medically necessary, the Contractor is responsible for Medicare cost sharing
if the member is a QMB dual, even if the Contractor determines the service is not
medically necessary. If Medicare denies a service for lack of medical necessity, the
Contractor must apply its own criteria to determine medical necessity. If criteria support
medical necessity, then the Contractor shall cover the cost of the service for QMB Duals.
D. PART D COVERED DRUGS
For QMB and Non-QMB Duals, Federal and State laws prohibit the use of AHCCCS
monies to pay for cost sharing of Medicare Part D medications.
RBHAs must utilize available Non-Title XIX/XXI funds to cover Medicare Part D
copayments for Title XIX/XXI and Non-Title XIX/XXI persons determined to have SMI,
with the following limitations:
Coverage of co-payments are to be used for medications on the AHCCCS
Behavioral Health Drug List,
Co-payments are to be covered for medications prescribed by RBHA in-network
providers,
RBHAs shall utilize Non-Title XIX/XXI funds for coverage of medications
during the Medicare Part D coverage gap, and
If a request for an exception has been submitted and denied by the Medicare Part
D plan and the coverage determination appeals process has been completed, the
RBHA may utilize Non-Title XIX/XXI funds to cover the cost of the non-covered
Part D medication for persons determined SMI, regardless of Title XIX/XXI
eligibility.
E. INSTITUTIONAL STATUS REPORTING – PART D COPAYS
1. Acute, RBHA, CMDP and CRS -- When a dual eligible member is inpatient in a
medical institution or nursing facility and that stay is funded by Medicaid for a full
calendar month, the dual eligible person is not required to pay copayments for their
Medicare covered prescription medications for the remainder of the calendar year.
(See Chapter 16b, Section 80.4.3 of the Medicare Managed Care Manual and
Medicare Prescription Drug Benefit Manual, Chapter 13, Section 60).
To ensure appropriate information is communicated for these members to CMS, the
Contractor must notify the AHCCCS, Member Database Management Administration
(MDMA), using the form provided in Attachment A of this Policy, as soon as it
determines that a dual eligible person is expected to be in a medical institution that is
funded by Medicaid for a full calendar month, regardless of the status of the dual
eligible person’s Medicare lifetime or annual benefits. Notification is to be submitted
as specified in Contract
. This includes:
a. Members who have Medicare Part “D” only,
b. Members who have Medicare Part “B” only,
c. Members who have used their Medicare Part “A” life time inpatient benefit, and

AHCCCS CONTRACTOR OPERATIONS MANUAL
CHAPTER 200 - CLAIMS
201 - Page 8 of 8
d. Members who are in a continuous placement in a single medical institution or any
combination of continuous placements in a medical institution.
2. Types of Medical Institutions -- For purposes of the medical institution notification,
medical institutions are defined as:
a. Acute hospitals,
b. Psychiatric hospital – Non IMD,
c. Psychiatric hospital – IMD,
d. Residential treatment center – Non IMD,
e. Residential treatment center – IMD,
f. Skilled nursing facilities, and
g. Intermediate Care Facilities for the Intellectually Disabled.
ALTCS/EPD and DDD are not required to provide this information as the State is
already aware of the institutional status of these members and provides this
information to CMS.



