Fillable Printable Payment Modernization Plan Sfy2014
Fillable Printable Payment Modernization Plan Sfy2014
Payment Modernization Plan Sfy2014
AHCCCS Payment Modernization Plan
SFY 2014
Introduction
Arizona Health Care Cost Containment System (AHCCCS), the State’s Medicaid Agency, uses
Federal, state, and county funds to provide health care coverage to the State’s acute and long-
term care Medicaid population and other qualified low income Arizonans. AHCCCS was
established as a mandatory managed care program that makes prospective capitation
payments to contracted health plans responsible for the delivery of care. In State Fiscal Year
(SFY) 2014, AHCCCS is expected to spend approximately $9.5 billion, providing health care
coverage to over 1.3 million Arizonans through contracts with 11 different Managed Care
Organizations that depend on a network of over 55,000 providers.
Payment Modernization is a cornerstone of the Agency’s strategy to bend the upward
trajectory of health care costs. By building on the established AHCCCS managed care delivery
model, the intent is to reduce growth in per capita expenditures, and to improve members’
health outcomes. This Care delivery and payment system transformation will be achieved
through collaboration with Agency stakeholders.
The AHCCCS Payment Modernization Plan includes a discussion of the current healthcare
delivery and payment system, the framework for moving payment modernization forward, and
actions needed for successful system transformation.
Healthcare Delivery System Assessment
The Institute of Medicine 2012 report, “Best Care at Lower Cost” estimated that approximately
$750 billion of United States health care costs are wasted annually. The reasons include
unnecessary services, inefficient care, excessive administrative costs, inflated prices, prevention
failures, and fraud. Other health care system shortcomings include inconsistent care outcomes,
payment models which reward quantity instead of quality, and fragmented care transitions
among provider settings. Health care costs are projected to continue to consume an increasing
percentage of the nation’s economic output for the foreseeable future.
There is widespread agreement that the current rate of health care spending is not sustainable.
There is also general consensus (“Partnership for Sustainable Health Care”, Robert Wood
Johnson 2013; “Best Care at Lower Cost”, Institute of Medicine 2012; “National Commission on
Physician Payment Reform”, Society of General Internal Medicine 2013) about the changes
which must occur to establish a high value, financially sustainable health delivery system.
In recent years, there have been numerous initiatives attempted by government payers, health
systems, and providers across the country, including Arizona, to address the health care
system’s deficits. Some have been successful, but generally not on a large scale. Most experts
agree that aligning incentives among providers, managed care organizations (MCO’s), and
patients, results in better and less costly care. However, transforming our nation’s health care
system to be value based rather than transaction based has proven to be extremely
challenging. Medicare has attempted to improve care coordination and reduce cost by
instituting provider structures such as hospital readmission penalties, as well as demonstration
projects for concepts such as accountable care organizations (ACO’s) and bundled provider
payments. Managed care organizations including many in Arizona are developing models such
as Patient Centered Medical Homes with similar goals. Many state Medicaid programs are
transitioning to care delivery models similar to the AHCCCS managed care model, and moving
toward value based care delivery models in recognition that fee for service payment methods
are not sustainable. However, according to Catalyst for Payment Reform, a nationally
recognized independent organization whose mission is to accelerate healthcare payment
reform, currently only 11% of commercial health plan in network payments to providers
nationwide are value oriented, and not traditional fee for service.
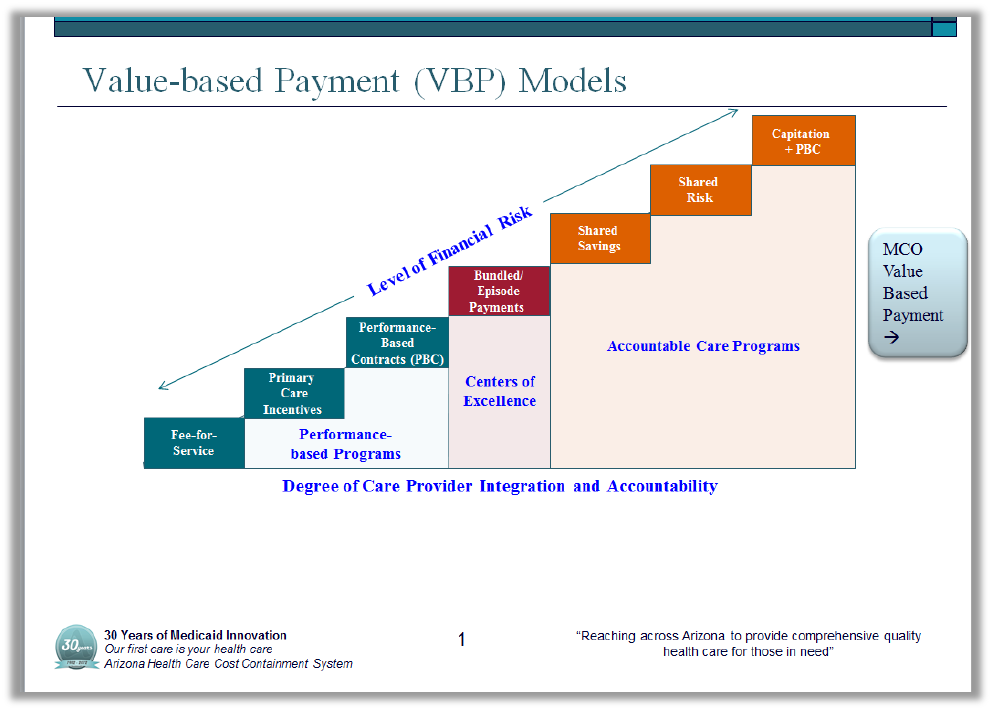
This chart shows a continuum of value based care and payment models. The continuum is
based on the degree of financial risk, integration, and accountability assumed by providers. The
models also vary by the degree to which there is accountability for care outcomes and overall
value. Transitioning from the predominant current Fee for Service model to the models with
greater levels of provider integration and accountability for outcomes is essential to payment
modernization.
Payment Modernization Mission
To leverage the AHCCCS managed care model toward value based health care systems where
patients’ experience and population health are improved, per-capita health care cost is limited
to the rate of general inflation through aligned incentives with managed care organization and
provider partners, and there is a commitment to continuous quality improvement and learning.
Payment Modernization Plan Foundation
AHCCCS has a long history as an innovator. Through the Payment Modernization Plan
the agency is committing resources to leverage the State’s successful managed care model to
address inadequacies of the current health care delivery system such as fragmentation, and to
continue to lead efforts to bend the health care cost curve to sustainable levels.
As one of the largest health care purchasers in the State of Arizona the AHCCCS Payment
Modernization Plan is grounded in three broad based goals.
1. AHCCCS must promote and facilitate a culture of learning and growth around payment
modernization both internally and externally
2. AHCCCS must leverage its position among Arizona healthcare payers to promote more
cost and outcome transparency in the healthcare delivery system.
3. AHCCCS must deploy a variety of strategies that leverage health plans and other
stakeholders resulting in more value based purchasing moving up the payment
modernization continuum
The AHCCCS Payment Modernization Plan provides a framework intended to guide policy to:
• Health care that is affordable and financially sustainable for taxpayers and members.
• A delivery system that is accountable for health outcomes and resource use.
• Patients who are informed, empowered, and engaged in their care.
• An environment that fosters a culture of continuous improvement and learning.
• Reliable information that can be used to monitor and transform quality, cost, and
population health.
• Patient care that is evidence-based and safe.
• Innovation and improvement through healthy competition based on cost, patient
experience, and health outcomes, with AHCCCS as an essential partner.
Establish a Culture of Learning
• Establish robust stakeholders’ input opportunities for health plans, providers and other
interested parties to identify and implement effective payment modernization
strategies.
• Establish baseline measurement of current value based medical spend by AHCCCS
contracted MCOs consistent with the payment modernization continuum presented in
Table 1. Update this measurement annually.
• Participate in, and leverage Catalyst for Payment Reform (CPR) and other organizations
which support and foster new value based payment models and drive payment
modernization strategies.
• Convene the AHCCCS Executive Management Team regularly to evaluate Payment
Modernization Plan implementation and to identify new opportunities.
• Work collaboratively with contracted MCO’s to reward high performing providers, and
support initiatives which move from fee for service payment models.
• Provide incentives for the use of evidence based innovative care models, particularly for
models which focus on paying for care which is proven to work.
• Support and drive data analytics development which enables MCOs to reduce care
fragmentation among providers and care settings.
• Monitor and accelerate MCOs’ use of incentives to providers such as gain sharing for
meeting benchmarks which improve patient safety, including hospital acquired
conditions, adverse drug events, and surgical site infections.
Expand Transparency
• Enhance the accessibility of information on cost, outcomes, and patient experience
which can be utilized to reward high performing providers and to help drive innovation.
• Make recommendations to the legislature by January 1, 2014 on strategies to improve
hospital charge master reporting to enhance charge and cost transparency
• Publish results to providers from episodic payment modeling to inform clinical
community on variation in reimbursement.
• Compare newly mandated reporting requirements as established by Laws HB2045 ,
Chapter 202 with other published documents like the charge master
• Work to increase the availability of payment, utilization, and cost information on the
AHCCCS website as well as highlight Payment Modernization initiatives.
FY 2013 Key Accomplishments
• The requirement for ALTCS MCOs to enter shared savings agreements with contracted
providers was expanded to the Acute Care procurement [Payment Reform Initiative].
Incentive payments are paid to health plans and providers who demonstrate improved
health outcomes and reduced costs.
• Contracted MCOs are required to identify how to improve alignment and integration of
care within their networks with identified cost reductions.
• The hospital inpatient reimbursement system is transitioning from a per-diem system to
a new methodology (APR-DRG) effective October 2014 which pays based on the
patient’s diagnosis and incentivizes hospitals to provide care more efficiently.
• The systems integration for the CRS, SMI, and Dual Eligible populations which are
underway will reduce care network fragmentation, align incentives, improve care
outcomes, and improve financial accountability.
• Executive level resources have been added to drive substantive system payment
modernization.
FY 2014 Initiatives
Payment Modernization Initiatives Underway
• Determining the ongoing structure and methodologies by which AHCCCS will further
incentivize, support, and prescribe the contracted MCOs’ adoption of value based
models of care delivery and payment, while continuing to foster MCO and provider
competitive innovation.
• Analyzing the shared savings criteria which will be established for future contracting
periods based on results of the Contract Year 2014 requirements for ALTCS and Acute
shared savings requirements.
• Implementing an E-prescribing initiative that seeks to leverage significant taxpayer
investment in Electronic Health Records.
• Facilitating process to develop a limited set of bundled payment structures to establish
greater reimbursement consistency for episodes of care within healthcare delivery
system.
• Implementing the new APR-DRG system by October 1, 2014.
• Support for increased development of patient centered care models which improve care
access and involve patients in their health decisions and options. Patient centered care
leads to better outcomes, lower costs, and an enhanced care experience.
• Leveraging and developing the Agency’s data analytics capabilities to enable effective
design, development and measurement of new care delivery models
Transforming healthcare delivery and payment models will be a long term process. The
transition from our current model must proceed with the interests of all stakeholders, most
importantly Arizona taxpayers and AHCCCS members, being aligned. Some actions can be
implemented more easily and quickly than others. AHCCCS and its MCO and provider partners
will move quickly with payment modernization where implementation and infrastructure
permits. This includes measures being implemented for the Payment Reform Initiative
beginning October 2013. Other more complex reforms will be undertaken more deliberately to
insure that significant measurable quality improvement and cost reduction progress is
achieved.
Through ongoing dialogue with key stakeholders and a commitment to continuous learning and
improvement, the AHCCCS Payment Modernization effort will continue to identify and
implement effective and sustainable initiatives which provide the highest possible value for the
Arizonans we serve.



