Fillable Printable Pcs Rates Vaccine Fa Qs
Fillable Printable Pcs Rates Vaccine Fa Qs
Pcs Rates Vaccine Fa Qs
1
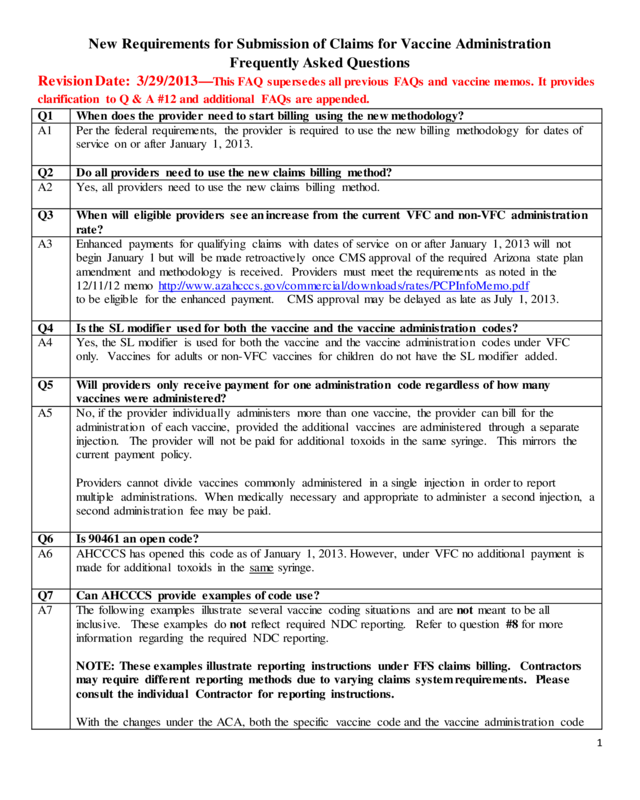
New Requir ements for Submissi on of Cl aims f or Vacci ne Admi ni str ation
Frequent l y Asked Quest i ons
Revision Date: 3/29/2013—
This FAQ supersedes a ll prev io us FAQs a nd v a cc ine memos. I t pro v ides
clarification to Q & A #12 and additional FAQs are appended.
Q1
When does the provider need to start billing using the new methodology?
A1
Per the federal requirements, the provider is required to use the new billing methodology for dates of
service on or after January 1, 2013.
Q2
Do all providers need to use the ne w cla ims billing method?
A2
Yes, all providers need to use the new claims billing method.
Q3
When will eligible providers see an increase from the current VFC and non-VFC administration
rate?
A3
Enhanced payments for qualifying claims with dates of service on or after January 1, 2013 will not
begin January 1 but will be made retroactively once CMS approval of the required Arizona state plan
amendment and methodology is received. Providers must meet the requirements as noted in the
12/11/12 memo
http://www.azahcccs.gov/commercial/downloads/rates/PCPInfoMemo.pdf
to be eligib le for the enhanced payment. CMS approval may be delayed as late as July 1, 2013.
Q4
Is the SL modifier used for both the vaccine and the vaccine administration codes?
A4
Yes, the SL modifier is used for both the vaccine and the vaccine adminis tratio n codes under VFC
only. Vaccines for adults or non-VFC vaccines for children do not have the SL modifier added.
Q5
Will providers only receive payment for one administration code regardless of how many
vaccines were administered?
A5
No, if the provider individually administers more than one vaccine, the provider can bill for the
administratio n of each vaccine, provided the additiona l
vaccines are administered through a separate
injection. The provider will not be paid fo r additional toxo id s in the same syringe. This mirrors the
current payment policy.
Providers cannot divide vaccines commonly administered in a single injection in order to report
multiple administrations. When medically necessary and appropriate to administer a second injection, a
second adminis trat io n fee may be paid.
Q6
Is 90461 an o pen c o de?
A6
AHCCCS has opened this code as of January 1, 2013. However, under VFC no additional payment is
made for additional toxoids in the same syringe.
Q7
Can AHCCCS provide examples of code use?
A7
The following examples illustrate several vaccine coding situations and are not meant to be all
inclusive. These examples do not reflect required NDC reporting. Refer to question #8 for more
information regarding the required NDC reporting.
NOTE: These examples illustrate reporting instructions under FFS claims billing. Contractors
may require different reporting methods due to varying claims system requirements. Please
consult the individua l Contractor for re porting ins tructions .
With the changes under the ACA, both the specific vaccine code and the vaccine administration code
2
must be reported by all providers reporting vaccine administration services.
• If the vaccine is provided through the VFC program, the SL modifie r must be a dded to bo th
the vaccine code and the vaccine administration code. Do not add the SL modifier to
vaccine and administr atio n codes used to report services provided to members who are 19 years
of age or older or for vaccines not covered under the VFC program administered to children.
• C PT c o d e s id e nti fy in g the va c c ine o r to xo id give n und e r t he VF C p r o gra m s ho uld be identified
with the appropriate CPT code to identify the vaccine, the SL modifie r, and the charge listed as
$0.00.
• Vaccines should be identified with the appropriate CPT code and the charge for that vaccine for
members 19 years of age or older or for vaccines not covered under the VFC program
administered to children.
Codes: 90460 & 90461
As no te d in Q5,
more than one vaccine administration payment can be made if multiple injections are
given to the member. Reporting multiple injections depends on which vaccine administration codes
are used to report the services. When more than one vaccine is administered with counseling to a
member 18 years of age or younger,
each single injection is reported with CPT administration code
90460 (first or only component of each vaccine or toxoid administered) a nd if covered under VFC, add
the SL modifier.
Providers will be paid a separate administratio n fee for each separate injection. If mo r e t han o ne
vaccine/toxoid is included in a single injection, the additional toxoids should be identified with the
appropriate CPT code and if covered under VFC, add the SL modifier. Adminis tra tio n of those other
components/toxoids may be identified with CPT code 90461 a nd if covered under VFC, add the SL
modifier.
AHCCCS will not make additional payment for administration of other additional toxoids included in
the injection identified with CPT code 90460. Providers are not compelled to report 90461 for the
administration of those additional toxoids.
Codes: 90471, 90472, 90473, 90474
W he n mo re tha n o ne inj ec tion is given to a me mb e r who is 19 years of age or older or to a
child without
counseling, the administration of the first injection is identified with CPT code 90471
and additional injections are identified with CPT code 90472. Each vaccine or toxoid component
should be identified with the appropriate CPT code on the claim form along with the charge for that
toxoid. Intranasal or oral administration should likewise be coded with CPT code 90473 and additional
administrations are identified with CPT code 90474.
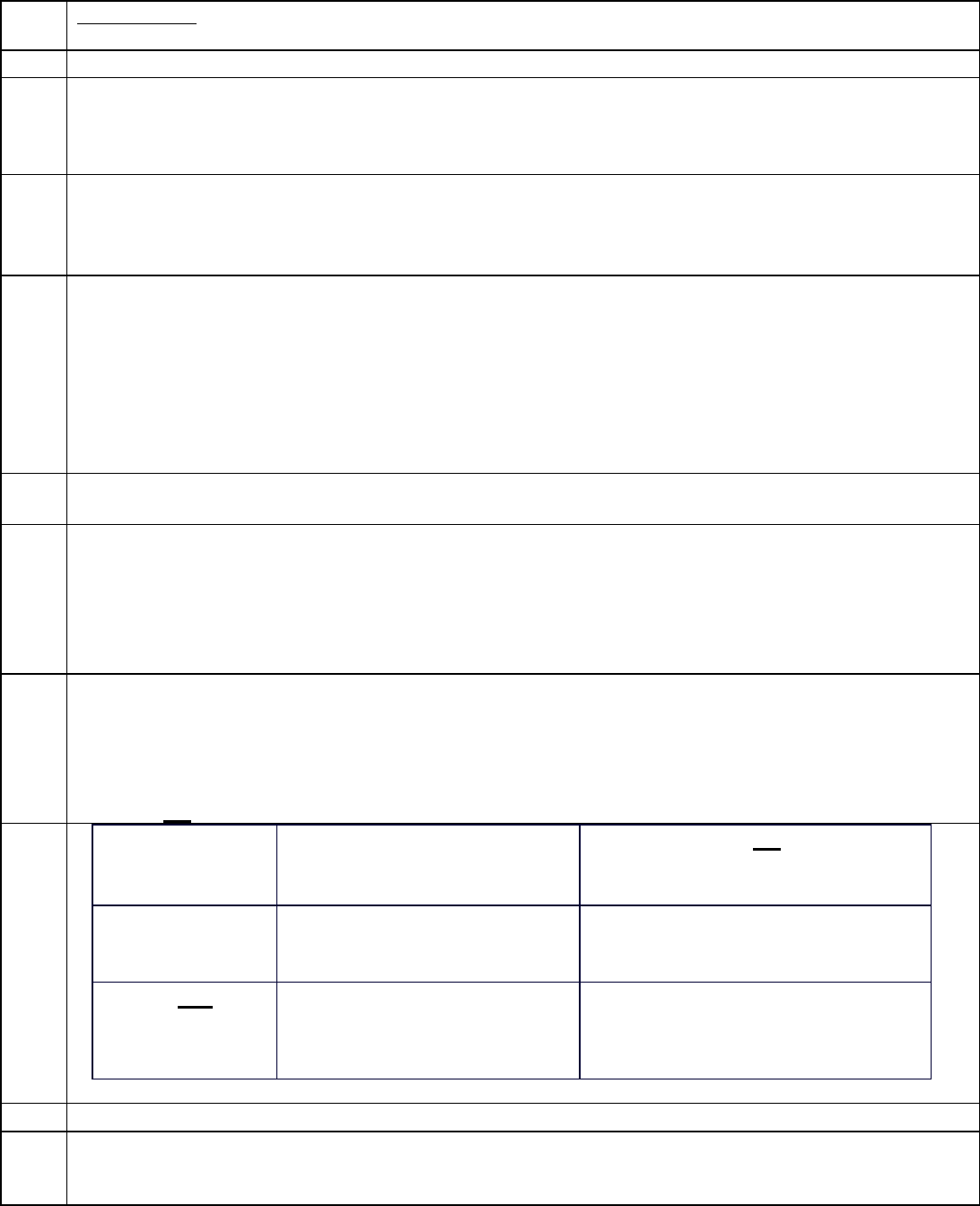
Example 1: Child 18 years of age or under receiving one VFC injection
24. A B C D E F G
Dates of Service Place of Service EMG
Procedures, Services or
Supplies
Diagnosis
Poi nte r
$ Ch a rges Uni ts
1/1/13-1/1/13 11 90460 SL 1 $xx.xx 1
1/1/13-1/1/13
11
90700 SL
1
0.00
1
3
Example 2: Child 18 years of age o r under receiving three separate VFC injections
24. A
B
C
D
E
F
G
Dates of Service
Place of Service
EMG
Procedures, Services or
Supplies
Diagnosis
Poi nte r
$ Ch a rges
Uni ts
1/1/13-1/1/13
11
90460 SL
1
$xx.xx
3
1/1/13-1/1/13
11
90700 SL
1
0.00
1
1/1/13-1/1/13 11 90655 SL 1 0.00 1
1/1/13-1/1/13 11 90707 SL 1 0.00 1
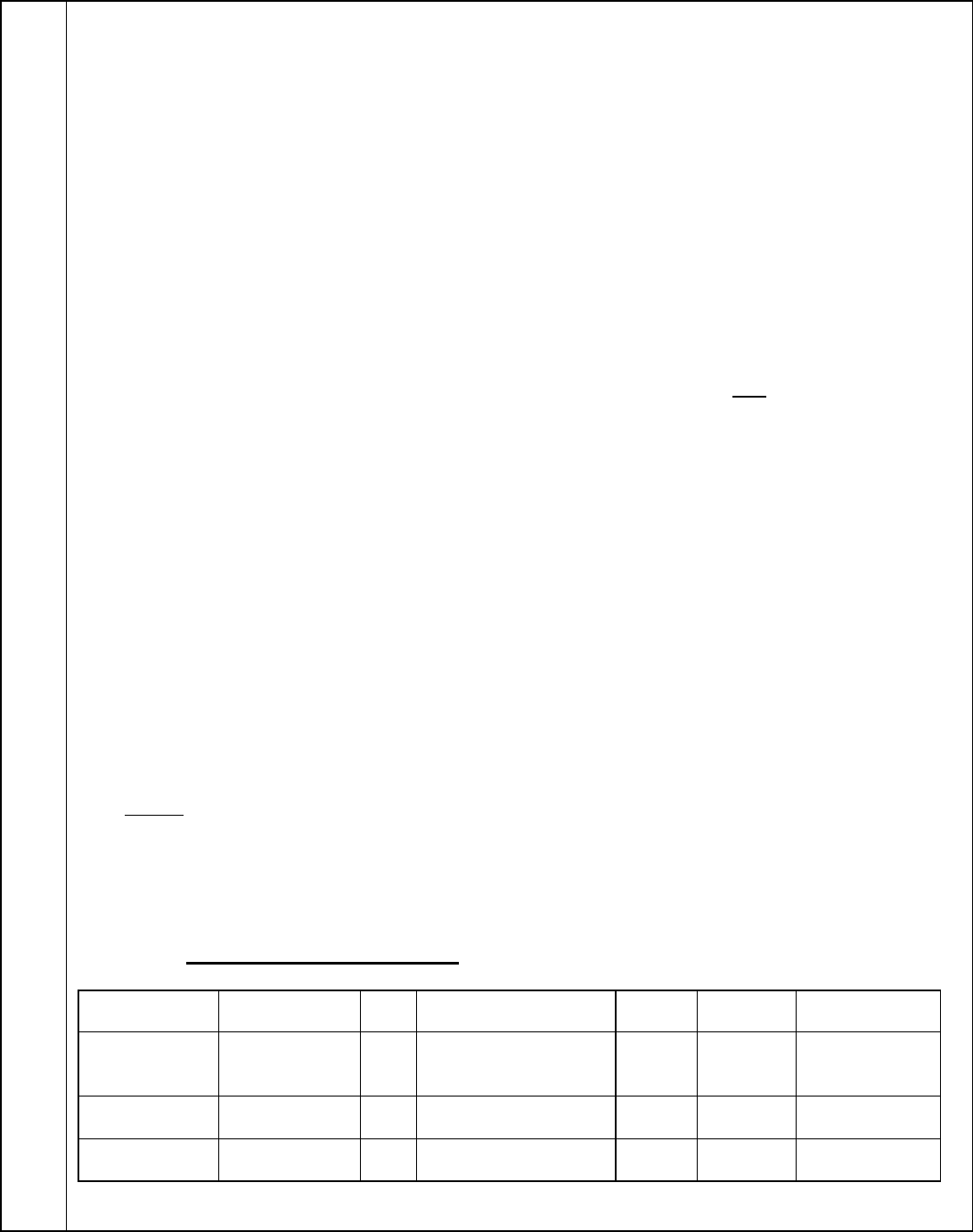
Note: Examples 3 and 4 would also apply to non-VFC i njec ti ons fo r chi ldren.
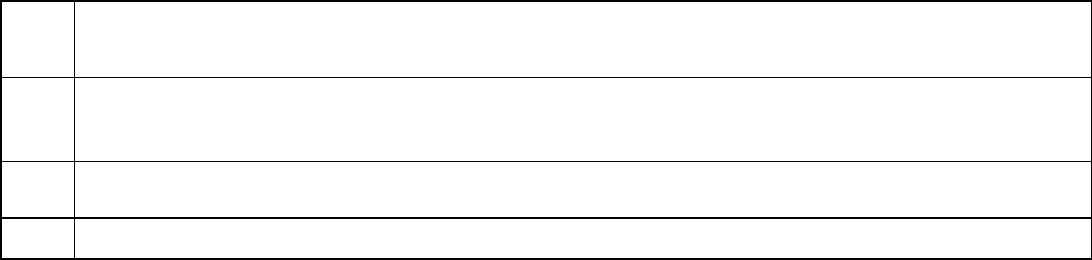
Example 3: Member 19 years of age or older
receiving one injection
24. A B C D E F G
Dates of Service
Place of Service
EMG
Procedures, Services or
Supplies
Diagnosis
Poi nte r
$ Ch a rges
Uni ts
1/1/13-1/1/13
11
90471
1
$xx.xx
1
1/1/13-1/1/13 11 90656 1 $xx.xx 1
Example 4: Member 19 years of age or older
re ceiving three injections
24. A
B
C
D
E
F
G
Dates of Service
Place of Service
EMG
Procedures, Services or
Supplies
Diagnosis
Poi nte r
$ Ch a rges
Uni ts
1/1/13-1/1/13
11
90471
1
$xx.xx
1
1/1/13-1/1/13
11
90472
1
$xx.xx
2
1/1/13-1/1/13
11
90656
1
$xx.xx
1
1/1/13-1/1/13
11
90670
1
$xx.xx
1
1/1/13-1/1/13 11 90703 1 $xx.xx 1
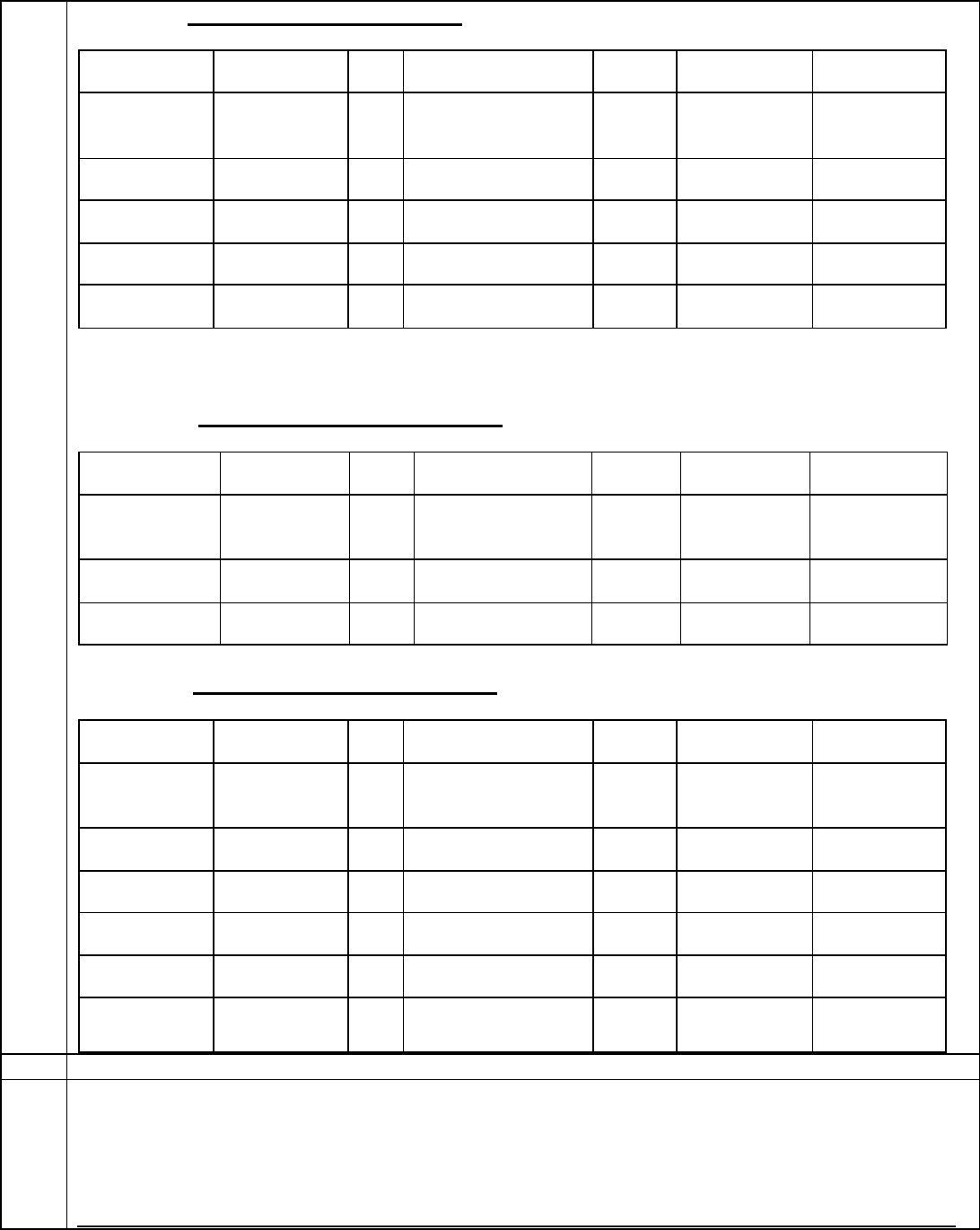
Q8
Is the NDC required when billing VFC and non-VFC vaccine s e rvice s?
A8
Yes the NDC is required. The current billing standards for reporting NDC information on the
Professiona l claim form for AHCCCS are consistent with the instruct io ns and standards for the
CMS1500 form as published by NUCC. To the extent an NDC is appropriate to report, the other
related data elements are also required by the form and the policy we have adopted.
Refer to the pharmacy web page at:
http://www.azahcccs.gov/commercial/Downloads/PharmacyUpdates/NDCBillingRequirementsFAQs_
4
Additional.pdf for additional information specific to NDC usage.
Q9
Are G0008, G0009 and G0010 administration codes el ig ible f o r the enha nc ed ra te?
A9
No t hey a r e no t . Unde r 42 CFR 447. 400, only CPT codes 90460, 90461, 90471, 90472, 90473 and 90474
or their successor codes are eligible for the enhanced rate. Note that these codes are eligible for the
enhanced ra te only if the y are ope n code s within the State Medicaid program.
Q10
Recently several specialty societies issued guidance directing providers reporting vaccine and
vacci ne admin istr ati on ser vices on th e same d ate of ser vice as an Evalu ation and Man agement
(E&M) service, including Preventive Medicine exams, to add Modifier 25 to the E&M code. Do
the se ins tructions apply to claims submitte d to AHCCCS?
A10
CMS has added numerous code pairs to the Correct Coding Initiative (CCI) list of codes Procedure to
Procedure code edits. These new edits, effective 1/1/13, pair the vaccine adminis tra tio n codes (90460,
90461, and 90471-90474) with the E&M codes. These CCI edits do not allow both the vaccine
administr ation service and the E&M service to be paid for the same date of service unless the E&M
service is identified with modifier 25. A HCCCS mu s t adopt thes e CCI edits. Providers administering
vaccines and performing an E&M service on the same date of service must add modifier 25 to the
E&M code. Modifier 25 is not added to the vaccine administration codes.
Q11
Will the AHCCCS VFC administrat ion rate increas e to the ne w regional max imum fo r a ll
providers?
A11
No. AHCCCS has elected not to adopt the new regional maximum VF C rate . Providers who are
eligib le for enhanced payment rates will receive the enhanced rate of $21.33 for vaccine adminis tratio n
under VFC.
For all other vaccine administrations under VFC, the AHCCCS rate of $15.43 remains unchanged.
Q12
What are the potential AHCCCS v ac cine VFC and non-VFC adm inistr ation rates for eligible
and non-eligible phys icians for CY 2013 and 2014 once AHCCCS gains approval for the ir State
Pla n Amendment a nd metho do lo g y ?
Note: This s imple chart is inte nde d only to illus trate the reimbursement difference between
ACA-eligible and non-eligible providers, as well as bet ween VFC a nd no n-VFC administration
and doe s not provide for all continge ncie s.
A12
Example
Physician eligible
fo r enha nc ed f ees
Physician not eligible
for e nhance d fe es
Va cc ine pro v ided
through VFC
$21.33 / each separate injection
$15.43 / each separate injection
Vaccine not provi
ded thro ug h VFC
$26.81 / each separate injection
plus fee for vaccine/to xo id
$20.64 / each separate injection
p lus fe e for vaccine/toxoid
Q13
Can 90460 be us e d if the RN is giving the inje ction to a child?
A13
As lo ng a s the physician has counseled the member, 90460 may b e us e d w hen the nur se ha s give n the
injection.
5
Q14
For an adult, when there is a ser ies of three immuniz ations, the doctor consult s at the point of the f irst
immunization. W hen the member comes back f or the 2
nd
and 3
rd
inj ection and the RN gives the inj ection
does the nurse use 90471?
A14
The use of the code is dependent on whether or not the p hys ic ian ha s d o ne fo llo w up c o unse l in g to the
member.
Q15
If the physician administers multiple vaccine injections on the same day, will s/he be paid the
same administration rate for each injection?
A15
Yes the reimburse me nt rate will be the same for each administratio n of the injectio n.



