Fillable Printable Program Integrity Plan
Fillable Printable Program Integrity Plan
Program Integrity Plan
AHCCCS Program Integrity Plan 2016 Page 1 of 4
AHCCCS PROGRA M INTEGRITY PLAN
2016
INTRODUCTION
Arizona Health Care Cost Containment System (AHCCCS), the State’s Medicaid Agency, uses
federal, state, and county funds to provide health care coverage to the State’s low income groups,
acute, and long-term care Medicaid population. AHCCCS was established as a mandatory
managed care program that makes prospective capitation payments to contracted health plans
responsib le for the de livery of c are. In 2016, AHCCCS is expected to spend approxim ately $11.23
billion providing health care coverage to over 1.8 million Arizonans through a network of over
61,000 providers.
The Centers for Medicare and Medicaid (CMS) policy defines Medicaid Program Integrity as the
“…planning, prevention, detection, and investigation/recovery activities undertaken to minimize or
prevent o verpa yments due to Me dicaid f raud, waste, o r abuse.” In keepi ng with the c om prehensi ve
nature of this definition, AHCCCS believes that Program Integrity is an important component of all
operational departments. Program Integrity is also an important piece of the overall
agency
Strate g ic Pla n .
ENVIRO N MENTAL SC AN or SITUATIONAL ASS ES SMENT
AHCCCS c ontinues to eva luate and im plement Program Integrity strategies to address the gr owing
number of Arizonans receiving Medicaid.
AHCCCS c ontinues to f ocus on the integration of physical and behavior al health. In 2015, thr ough
collaborat ion with the Arizo na Department of H ealth Services, m em bers with Ser ious Mental Illness
in the greater par t of Ari zon a wer e trans it ion ed to a s in gle plan to inte gr ate b oth p h ysica l and mental
health serv ices. This proces s occurred in Maricop a County in 2014, al lowing this year’s integration
of services to be available statewide. In addition, over 85,000 Dual Eligible AHCCCS members
began receiving physical health, general mental health, and substance abuse services from their
single acute health plan.
AHCCCS c ontinues to ex pand on proc esses related to Payment M odernization. AHCCCS and our
contracted plans are spending considerable time and effort on strategies to move away from a
traditional fee-for-service arrangement to better aligned reimbursement systems. AHCCCS
continues to increase requirements on our contracted plans in terms of value based payment
structures. These requirements will continue to escalate in the future.
Addition al ly, AHCCCS co nt inu es to b e i nv ol ved in ef f orts nati ona ll y b y Med icai d D i r ec tors to eng age
CMS on establishing m ore collaborative, focused, and efficient program integrity efforts. Given the
changing landscape of the entire healthcare system and the challenges associated with
implementation of new mandates, the AHCCCS Administration is developing the 7
th
Annual
Program Integrity Plan. The plan summarizes previous accomplishments and identifies new
strategies to ensure the best possible use of limited resources.
Given the current fiscal environment at both the state and federal level, and the size of the
AHCCCS program, Program Integrity efforts are critical if maximum dollars are to remain available
to serve individuals in need.
PROGRAM INTEGRITY MISSION
Throughout the Agency, promote economy, efficiency, accountability, and integrity in the
management and delivery of services in order to ensure that AHCCCS is an effective steward of
limited resources.
CY 2015 K EY ACCO M PLISHM ENT S
AHCCCS realized over $1 billion in avoided and recovered costs as a result of coordination of
benefits, third party recoveries, and Office of the Inspector General (OIG) activities.
AHCCCS supported the investigations of 27 successful prosecutions of either members or
providers.
AHCCCS Program Integrity Plan 2016 Page 2 of 4
AHCCCS receives data from Motor Vehicle Division (MVD) and Industrial Commission to assist
with third party liabi lity ide nt ifica tio n .
AHCCCS receives County inmate data for more than 80% of the state to assist with eligibility
compliance.
AHCCCS established a non-emergency medical transportation (NEMT) task force to develop
more robust strategies and change policies to strengthen provider oversight. The screening
process including site visits and routine checks through the PECOS database has started and
will continue throughout the 2016 calend ar year.
Civil Monetary Penalties were issued in CY 2015 amounting to $5,860,517.25 in s anct ions.
5 provider suspensions were issued during FY 2015 as a result of the determination of credible
allegations of fraud.
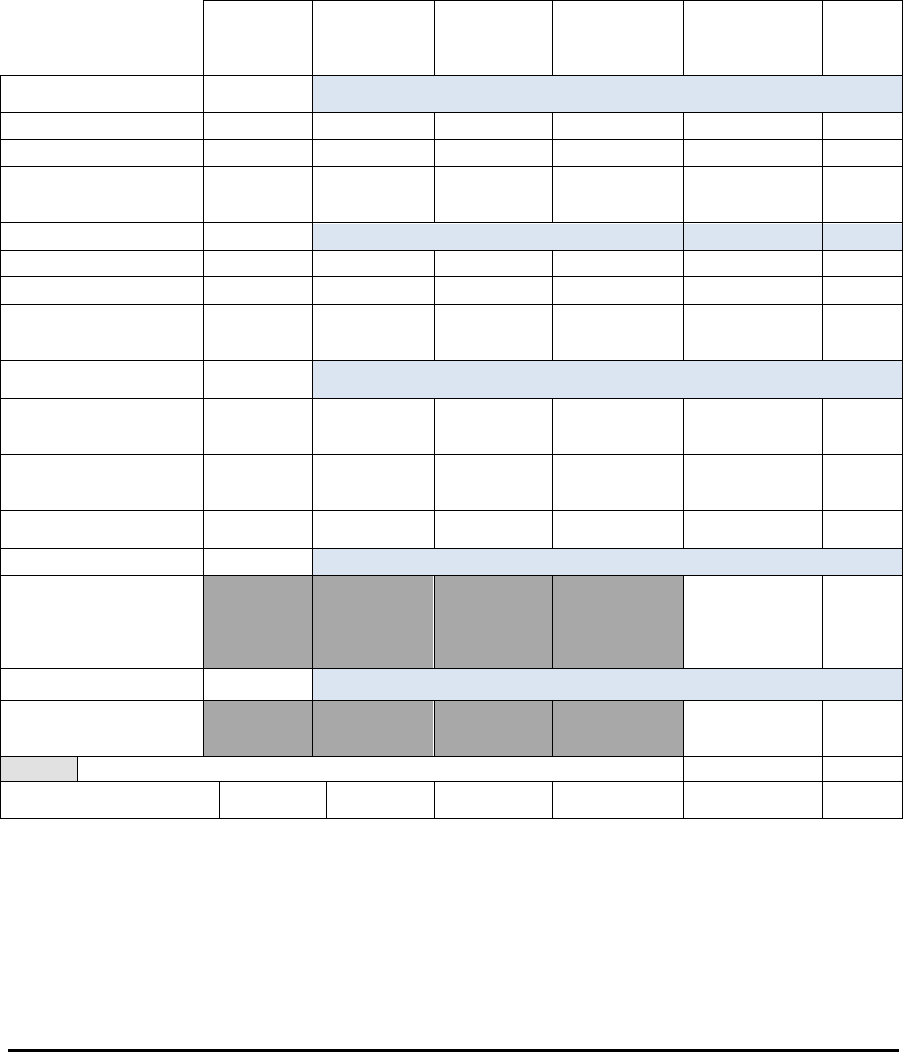
AHCCCS Recovery, Savings and Cost Avoidance
SFY 2011 SFY 2012 SFY 2013 SFY 2014 SFY 2015
%
Change
SFY14-
SFY15
Coordination of
Benefits
Total Commercial COB
$113,001,472 $112,038,407 $121,716,277 $ 125,064,195 $140,400,878 +12%
Total Medicare COB *
$815,066,365 $836,709,557 $922,490,575 $ 1,055,239,043 $991,531,425 -6%
Total COB
Cost
Avoidance
$928,067,837 $948,747,964 $1,044,206,851 $ 1,180,303,238 $1,131,932,303 -4%
Third Party Liability
Total Recoveries **
$9,924,206 $11,118,940 $11,692,628 $ 11,905,088 $8,843,418 -26%
Total Distri butions
$8,310,570 $9,232,308 $9,427,596 $ 9,976,724 $7,348,805 -26%
Net
Recoveries
fro m TP L
$1,613,636 $1,886,632 $2,265,032 $1,928,364 $1,494,613 -22%
Office of Inspector
General (OIG)
Provider Fraud Unit
Recoveries and
Savings***
$6,007,659 $11,094,794 $19,200,500 $24,033,483
$11,934,312
-50%
Member Fraud Unit
Recoveries and
Savings****
$24,493,145 $29,967,560 $31,712,316 $34,217,415 $26,210,174 -23%
Total OIG
Recoveries
$30,500,804 $41,062,354 $50,912,816 $58,250,898 $38,144,487 -35%
Incarceration No Pay+
Incarceration
Total
Capitation
Cost
Avoided
$26,006,071
N/A
FFS Audit Savings+
Total FFS
Audit
Savings
$2,366,468.14
N/A
RECOVERY/COST
AVOIDANCE T OTAL
$960,182,277 $991,696,950 $1,097,384,699 $1,240,482,500 $1,199,943,942 -3%
* Excludes i dentified reporting errors; SFY 2011 includes 2 previously excluded MCOs
** I ncludes estate, trust, and casualty recoveries for fee-for-service and joint case reinsurance payments
*** Report of Provider Fraud Unit results (includes global settlem ents & Savings)
**** Report of Member Fraud Unit results (includes Social Sec urity leads)
+ Added to this report in FY2015

AHCCCS Program Integrity Plan 2016 Page 3 of 4
2016 PROGRAM INTEGRITY STRATEGIES
1. Automation
a. Provider Automation
i. Developing an on-Line Provider Registration process
ii. Creating an on-Line Pro vider abilit y to update their file inf ormation
b. Collecti on’s Port a l
i. Set forth ACH payment options for Providers and Members related to approved
settlement agreements
c. DHS Licenses
i. Automation of licensing data interface directly with AHCCCS data for provider
verification
d. Case Tracking Platform
I. OIG is deploying resources to develop a document repository system to
store critical case information and develop more useful metrics
2. Data Analytics and Trends
a. OIG has been working closely with AdvanceMed (CMS contractor) in developing a system
that integrates Med icar e an d Medica id data to prov ide c as e information and inves t igat io n
development.
b. OIG will continue to pursue Program Integrit y Audits to follow-up on several that have been
completed to date including, Status B Codes, New Patient Billing, Dupl icat e E&M and
Bilateral coding.
c. OIG will continue to partner with other stakeholders to develop reports from the new
eligibility HEAplus to ensure member compliance.
3. Partnerships
a. Improve collaboration with contractors under Corporate Compliance
I. Continue regular m eetin gs to shar e inf ormation with Managed Care Organizations
regarding their corporate compliance plan that includes all the program integrity
activities.
b. OIG will continue operating a task force with some of our most experienced investigators to
increase our footprint among law enforcement agencies.
c. OIG has broadened its resources by entering into a Memorandum of Understanding with
the Social Securi t y Adm inis tr atio n, which allows the OIG to identify and investigate referrals
pertaining to eligibility fraud.
d. OIG will work to ensure appropriate compliance with the new Hospital Presumptive
Eligibility program mandated by CMS.
e. OIG will continue to participate at the National Advocacy Center providing diverse trainings
to other states as well as ensuring participation from our work force.
f. OIG will continue to actively partner with other states to strengthen resources and
knowledge.

AHCCCS Program Integrity Plan 2016 Page 4 of 4
g. OIG will partner with the Department of Public Safety (DPS) to run background checks on
high risk providers as required by CMS.
h. Participate in the Technical Advisory Group and the National Association of Medicaid
Directors meetings.
4. Non-Emergency Medical Transportation (NEMT) Tas k Force
a. Expand provider registration verification including:
I. OIG will regularly monitor FFS utilization of NEMT services for various provider
types.
II. OIG will continue to maintain current information on the website as it relates to
NEMT providers with active tribal business licenses.
b. AHCCCS will publish a Request for Information to tribal representatives to gather
information about the infrastructure available among tribes to administer an NEMT Broker
model.
c. OIG will continue to pursue permission from CMS to leverage the federal database PECOS
for provider information.
5. Program Integrity Operations
a. Continue emphasis on Program Integrity training
i OIG will continue to provide training and actively participating in task force
meetings, other agencies’ fraud related meetings and training.
ii OIG will continue to provide internal training for New Employees as well as
educating contractors and senior leadership on program integrity initiatives.
iii Provider Subject Matter Experts to provide training at the Department of Justice.
b. Continue expanding effective use of the Civil Monetary Penalties to enforce program
compliance.
c. Ensure the diligent use of the Credible Allegation of Fraud suspension process.
d. DFSM will continue to pursue and complete audits of payments made to providers.
6. Best Practices
a. Continue to enh ance and improve the subject matter topics for the Compliance Officer
Networking Group (CONG).
b. Creating an automated referral process to allow the OIG to track, monitor, and facilitate
appropriate and necessary case development.
c. Participate in the Global Settlement process.



